Stress Fracture Blog
Stress fractures are common overuse injuries that account for 50% of all injuries sustained by runners.1 The underlying cause has been shown to be linked to an accumulation of mechanical forces transmitted to the bone, eventually exceeding the repair and remodeling process of the bone.2 The bone is ultimately unable to withstand the repetitive loading, resulting in structural fatigue and localized bone pain and tenderness.3
The incidence of stress fractures in athletes varies according to sport. Track and field athletes have the highest incidence rates of lower extremity fractures – as high as 20%.4 Between ½ and 2/3 of competitive cross-country and long-distance runners have a history of a bone stress injury (BSI).5 35-49% of stress fractures in runners occur along the shaft of the tibia (shin bone) with others occurring in the femur (Thigh bone), fibula, calcaneus (heel), and the bones of the foot (metatarsals and tarsals).6
Of particular concern is the high recurrence rate of these injuries.
Up to half of track-and –field athletes with a history of BSI report sustaining a subsequent BSI within 1 to 2 years of their initial injury.7 Ultimately, the location and recurrence of a stress fracture is dependent on how an individual loads their skeleton when running.
Injury Mechanism
A stress fracture represents the inability of a bone to withstand repetitive mechanical loading. Excessive and repetitive loading of normal bone without sufficient rest time results in greater bone break down and does not allow for optimal time for recovery/new bone formation. Stress injuries represent a spectrum of injuries ranging from periostitis – inflammation of the bones outer lining (or periosteum) – to the development of tiny micro-fractures leading to observable swelling/edema within the bone (known as a stress reaction) – to a complete stress fracture that includes a cortical break.8 9
A stress reaction is the precursor to a stress fracture.
Throughout this progression, the boney structure is breaking down and becoming weaker. Once this process begins, if the repeated submaximal loading continues unchanged and without sufficient rest, a stress reaction may progress to a stress fracture (where there is a discernible fracture line within the cortical bone) and potentially even a full fracture.10
Risk Factors
There are many variables that can lead to stress fractures, which is part of the reason why they can be so difficult to treat. The management of these factors is key to successful long-term outcomes.
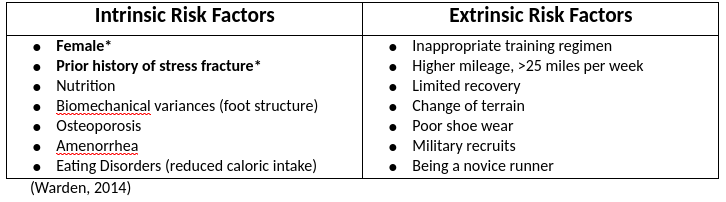
The 2 biggest risk factors include history of a stress fracture and the female gender.
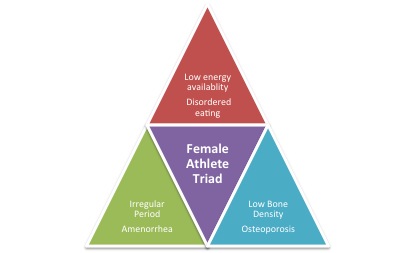
Females are generally at a greater risk for stress fracture and are commonly seen to demonstrate what is known as the Female Athlete Triad. This is an interrelationship of menstrual dysfunction (amenorrhea), low energy availability (with or without disordered eating) and reduced bone mass density (osteopenia) that is often seen in female athletes.11 This is often difficult to treat and requires a multidisciplinary approach.
Symptoms
Stress fractures most often evolve with an insidious onset that typically begins with pain/soreness occurring at the end of physical activity and may result with a focal point of tenderness.12 Typically, the pain is described as a mild diffuse ache that occurs after a specific amount of running or during a specific time of the gait cycle. Pain often does not resolve after a warm-up (although it can reduce), and as a run continues it tends to worsen and only abates once running or weight bearing has ceased.13
For most locations, a physical examination will demonstrate tenderness over the involved bony area – even when symptoms are felt as ‘diffuse’, a proper examination will often reveal a more focal region of tenderness.
Additional symptoms may include referred pain to joints above and below the site of fracture, focal swelling, and night pain.14
Diagnosis
Ultimately, a stress fracture can present with a multitude of symptoms therefore making it difficult to diagnose. During an evaluation an in-depth history will be taken to determine possible external and internal risk factors that may be attributing to the new onset of symptoms. Physical examination includes localized palpation of the bone, assessing for tenderness, callus formation, swelling or warmth of the tissue. Note – In some locations, palpation may not be possible (i.e. spine, femoral head) and alternative bone-loading tests will be utilized.15
Plain radiographs (X-ray) remain the first line of imaging due to the low cost and wide availability, however they can often miss an acute (new) stress fracture. An MRI is the gold standard largely due to its ability to display both soft tissue and bone edema.16
A bone scan may also be utilized; however, they are used less commonly due to radiation exposure.17
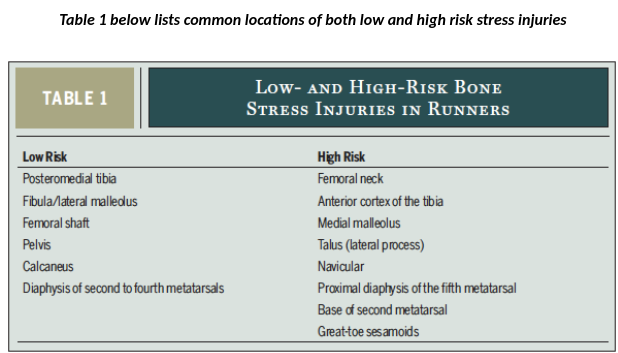
The diagnosis of a stress fracture can be categorized as either low and high risk. Low risk fractures occur on the compression side of the bones bending axis and have a favorable natural history with low incidence of complications.18 There is no need for aggressive intervention, surgery, or prolonged modified weight bearing.19 High risk fractures occur on the tension side of a bone’s bending axis and have treatment challenges that demand specific attention.20 So-called ‘high risk’ stress fractures are at elevated risk of delayed union or non-union and present a higher risk for progressing to a complete fracture.
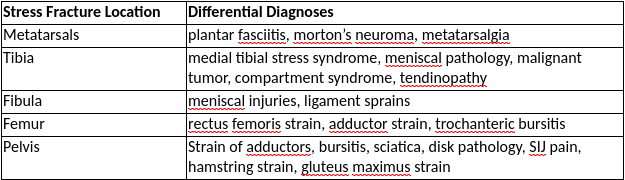
Differential Diagnosis
Multiple alternative diagnoses may be possible depending on the location of the stress fracture. In general, other diagnoses to consider include, compartment syndrome, tendinopathy, malignancies, or a nerve/ artery entrapment syndrome.21 The chart below indicates various stress fractures based on location and appropriate differential diagnoses to consider.
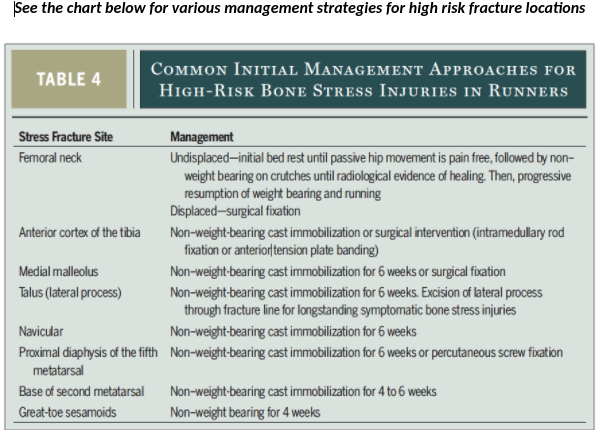
Treatment – High Risk Fracture Sites
These injuries are often difficult to diagnose resulting in delays in diagnosis and a risk of delayed union or nonunion, potentially resulting in progression to a complete fracture.
If the fracture does not require surgical fixation, the initial management approaches usually include a period (4-6 weeks) of non-weight bearing immobilization in a cast or boot.22 Duration weight bearing status is dependent on location of fracture, amount of cortical involvement, evidence of natural healing, and duration of symptoms.
Consideration for surgical intervention is highly dependent on fracture site. Surgical intervention may include fixation pins, screws, and/or plates to hold bones together during the healing process.23 Bone grafting is also possible for non-healing fracture sites.
Treatment – Low Risk Fracture Sites
Low Risk fractures sites are primarily treated with conservative care (Physical Therapy). Initially activity modification is necessary to allow for tissue healing, using pain (in part) as a principal guiding variable. If there is pain and abnormal mechanics with ambulation, non-weight bearing or use of a walking boot may be recommended.24 Night pain is often a sign of inflammatory involvement and is a good indication of overloading the bone.25
Nonsteroidal anti-inflammatory drugs are discouraged beyond a few days given their ability to mask pain and the potential to impede tissue-level healing.26
Key to recovery is identifying the risk factors that are placing undue load on the bone. This includes an in-depth history of general health, prior level of activity/training, history of previous overuse injuries medications used, personal habits, BMI, dietary patterns, maternal family history, lower extremity alignment, running mechanics, and shoe-wear.27
Identifying aspects of a patients’ history that places increased load on the bone must be identified and modified. This is then followed by interventions to improve the ability of the athlete to dissipate impact forces and improve the bone’s ability to resist loads.
Modifying loads:
Load management refers not only to reduced training volume, but also to addressing / eliminating training errors such as inappropriate progression of speed or duration, and insufficient / ineffective recovery (Specific strategies can be discussed with your PT).
Improving a muscles ability to absorb impact forces and reduce load transmitted up the leg can also be of great value. If muscles are weakened, fatigued or demonstrate altered activation patterns their ability to attenuate load becomes compromised.
Biomechanical factors such as foot structure, leg length discrepancies, and other anatomical abnormalities may be addressed with specific interventions.28 Lastly, addressing shoe-wear and running surface may also be necessary to improve attenuation of load.
Improving bones ability to resist loads:
3 modifiable factors that may impact the ability of the bone to resist loading and ultimately reduce stress fracture risk include – training history, energy availability, and calcium/vitamin D status.29
A longer history of training /physical activity is protective against the development of a stress fracture. The skeleton responds and adapts to mechanical loading in a site-specific manner in order to increase bone health and it’s ability to accept loads. Increasing bone mass by mechanical loading results in increased fatigue-resistance.30
Energy availability is directly related to dietary intake and energy expenditure. Low energy availability appears to be a central factor of the female athlete triad, therefore alteration of diet and exercise will need to be considered as part of a comprehensive management plan.3132
Lastly, calcium and vitamin D can contribute to bone rigidity. Athletes should ensure sufficient calcium and vitamin D intakes with the recommended allowance of 1000 to 1300 mg a day.33
Prognosis
The earlier the patient seeks care and the sooner a diagnosis is made, the more likely it is that the pathology will respond quickly and favorably to conservative management.34 Low risk injuries typically take around 8 weeks for return to sport. High risk injuries are more variable and typically take between 14-24 weeks for return to sport.35
No stress fracture is the same, therefore treatment and recovery can vary greatly.
Factors that may negatively influence normal bone healing times include smoking, diabetes, poor nutrition, compromised underlying bone health, and endocrine disorders or dysfunction.36
Return to Sport/Running
The general idea for return to sport or return to running is to utilize a graduated loading program that is guided by an understanding of physiology and informed by pain levels.
The historical rule of thumb has been to gradually progress a running program by no more than 10% per week.37 For example, if a patient runs 20 miles a week, the following week they should run no greater than 22 miles. When a more conservative approach is indicated, 5% increase per week are commonly used. The use of cyclic training may also be appropriate in order to allow introduction of rest periods.38 These commonly used guidelines are generic and more individualized and nuanced approach is often helpful.
A return to running ‘program’ should be 100% tailored the athlete’s unique training history, physiology, performance goals, and the details surround the injury (location, duration, etc).
The use of anti-gravity treadmill training (ATT), and reduced-gravity treadmill training can also be utilized to allow a patient to run at higher intensities earlier during their recovery with lower bone loading, as long as proper mechanics can be maintained.39
If faulty mechanics remain, despite progressive loading this may hinder the healing process.
The use of accelerometers as biofeedback tools to reduce ground reaction forces and shock during running has been found to be beneficial.40 Reducing stride length has also been found to reduce ground reaction forces by reducing the vertical excursion and velocity. 41 Changing foot strike from heel to mid-foot and/or forefoot may be effective in shifting how load is absorbed by the runner’s lower body. Depending on the location of the stress fracture, this can be very helpful.42 However, the induction of running gait changes should not be taken lightly, as there is always a risk of a potential injury at an alternative site as loads are suddenly introduced to new, un-conditioned, locations.
Importantly, each athlete is different, therefore variation in the time frame and response/adaptation to load will not be consistent.43
Communication with coaches and support staff is essential in order to ensure an appropriate loading regimen and adequate recovery – including appropriate nutrition, hydration, sleep, active rest, relaxation strategies and stress management.44
Conclusion
The high recurrence rate of stress injuries indicates the need for a comprehensive approach to address each underlying factor. The recovery from a stress injury can be complex, and requires the guidance of a physical therapist to safely return patients back to their prior level of function.
The Sports Physical Therapists at VASTA are experienced in guiding the injured athlete to a full recovery, helping each patient to get back to the active lifestyle they know and love.
References
- Clansey A, Hanlon M, Wallace E, Nevill A, Lake M. Influence of tibial shock feedback training on impact loading and running economy. Med Sci Sorts Exerc.2014;46:973-981
2. Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
3. Hoglund L, Silbernagel K, Taweel N. Distal fibular stress fracture in a female recreational runner: a case report with musculoskeletal ultrasound imaging findings. IJSPT. 2015, 10;7:1050-1058
4. Kiel J, Kaiser K. Stress Reaction and Fractures. [Updated 2019 Jun 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507835/
5. Nazem TG, Ackerman KE. The female athlete triad. Sports Health. 2012;4(4):302‐311. doi:10.1177/1941738112439685
6. Kahanov L, Eberman LE, Games KE, Wasik M. Diagnosis, treatment, and rehabilitation of stress fractures in the lower extremity in runners. Open Access J Sports Med. 2015;6:87‐95. Published 2015 Mar 27. doi:10.2147/OAJSM.S39512
7. Patel, D, Roth M, Kapil N. Stress fractures: diagnosis, treatment, and prevention. American Family Physician. 2011; 83:1
8. Warden SJ. Prophylactic use of NSAIDs by athletes: a risk/benefit assessment. Phys Sportsmed. 2010;38:132-138. http://dx.doi.org/10.3810/psm.2010.04.1770
9. Deldicque L, Francaux M. Recommendations for Healthy Nutrition in Female Endurance Runners: An Update. Front Nutr. 2015;2:17. Published 2015 May 26. doi:10.3389/fnut.2015.00017
10. Crowell,H.P.,Milner,C.E.,Hamill,J.,Davis,I.S. Reducing impact loading during running with the use of real-time visual feedback. J.Orthop.SportsPhysTher. 2010;40:206–213.
11. Crowell H, Davis I. Gait retraining to reduce lower extremity loading in runners. Clin Biomech. 2011; 26;78-83
12. Soligard T, et al. How much is too much? (Part 1) international olympic committee consensus statement on load in sport and risk of injury. Br J Sports Med 2016;50:1030–1041. doi:10.1136/bjsports-2016-096581
- Clansey A, Hanlon M, Wallace E, Nevill A, Lake M. Influence of tibial shock feedback training on impact loading and running economy. Med Sci Sorts Exerc.2014;46:973-981
- Clansey A, Hanlon M, Wallace E, Nevill A, Lake M. Influence of tibial shock feedback training on impact loading and running economy. Med Sci Sorts Exerc.2014;46:973-981
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Hoglund L, Silbernagel K, Taweel N. Distal fibular stress fracture in a female recreational runner: a case report with musculoskeletal ultrasound imaging findings. IJSPT. 2015, 10;7:1050-1058
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Hoglund L, Silbernagel K, Taweel N. Distal fibular stress fracture in a female recreational runner: a case report with musculoskeletal ultrasound imaging findings. IJSPT. 2015, 10;7:1050-1058
- Kiel J, Kaiser K. Stress Reaction and Fractures. [Updated 2019 Jun 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507835/
- Kiel J, Kaiser K. Stress Reaction and Fractures. [Updated 2019 Jun 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507835/
- Nazem TG, Ackerman KE. The female athlete triad. Sports Health. 2012;4(4):302‐311. doi:10.1177/1941738112439685
- Kahanov L, Eberman LE, Games KE, Wasik M. Diagnosis, treatment, and rehabilitation of stress fractures in the lower extremity in runners. Open Access J Sports Med. 2015;6:87‐95. Published 2015 Mar 27. doi:10.2147/OAJSM.S39512
- Kahanov L, Eberman LE, Games KE, Wasik M. Diagnosis, treatment, and rehabilitation of stress fractures in the lower extremity in runners. Open Access J Sports Med. 2015;6:87‐95. Published 2015 Mar 27. doi:10.2147/OAJSM.S39512
- Kahanov L, Eberman LE, Games KE, Wasik M. Diagnosis, treatment, and rehabilitation of stress fractures in the lower extremity in runners. Open Access J Sports Med. 2015;6:87‐95. Published 2015 Mar 27. doi:10.2147/OAJSM.S39512
- Kahanov L, Eberman LE, Games KE, Wasik M. Diagnosis, treatment, and rehabilitation of stress fractures in the lower extremity in runners. Open Access J Sports Med. 2015;6:87‐95. Published 2015 Mar 27. doi:10.2147/OAJSM.S39512
- Hoglund L, Silbernagel K, Taweel N. Distal fibular stress fracture in a female recreational runner: a case report with musculoskeletal ultrasound imaging findings. IJSPT. 2015, 10;7:1050-1058
- Kahanov L, Eberman LE, Games KE, Wasik M. Diagnosis, treatment, and rehabilitation of stress fractures in the lower extremity in runners. Open Access J Sports Med. 2015;6:87‐95. Published 2015 Mar 27. doi:10.2147/OAJSM.S39512
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Patel, D, Roth M, Kapil N. Stress fractures: diagnosis, treatment, and prevention. American Family Physician. 2011; 83:1
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-7659
- Warden SJ. Prophylactic use of NSAIDs by athletes: a risk/benefit assessment. Phys Sportsmed. 2010;38:132-138. http://dx.doi.org/10.3810/psm.2010.04.1770
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Deldicque L, Francaux M. Recommendations for Healthy Nutrition in Female Endurance Runners: An Update. Front Nutr. 2015;2:17. Published 2015 May 26. doi:10.3389/fnut.2015.00017
- Nazem TG, Ackerman KE. The female athlete triad. Sports Health. 2012;4(4):302‐311. doi:10.1177/1941738112439685
- Nazem TG, Ackerman KE. The female athlete triad. Sports Health. 2012;4(4):302‐311. doi:10.1177/1941738112439685
- Deldicque L, Francaux M. Recommendations for Healthy Nutrition in Female Endurance Runners: An Update. Front Nutr. 2015;2:17. Published 2015 May 26. doi:10.3389/fnut.2015.00017
- Deldicque L, Francaux M. Recommendations for Healthy Nutrition in Female Endurance Runners: An Update. Front Nutr. 2015;2:17. Published 2015 May 26. doi:10.3389/fnut.2015.00017
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Kahanov L, Eberman LE, Games KE, Wasik M. Diagnosis, treatment, and rehabilitation of stress fractures in the lower extremity in runners. Open Access J Sports Med. 2015;6:87‐95. Published 2015 Mar 27. doi:10.2147/OAJSM.S39512
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Warden S, Davis I, Frederickson M. Management and prevention of bone stress injuries in long-distance runners. JOSPT. 2014;44:749-765
- Crowell,H.P.,Milner,C.E.,Hamill,J.,Davis,I.S. Reducing impact loading during running with the use of real-time visual feedback. J.Orthop.SportsPhysTher. 2010;40:206–213.
- Crowell,H.P.,Milner,C.E.,Hamill,J.,Davis,I.S. Reducing impact loading during running with the use of real-time visual feedback. J.Orthop.SportsPhysTher. 2010;40:206–213.
- Crowell H, Davis I. Gait retraining to reduce lower extremity loading in runners. Clin Biomech. 2011; 26;78-83
- Soligard T, et al. How much is too much? (Part 1) international olympic committee consensus statement on load in sport and risk of injury. Br J Sports Med 2016;50:1030–1041. doi:10.1136/bjsports-2016-096581
- Soligard T, et al. How much is too much? (Part 1) international olympic committee consensus statement on load in sport and risk of injury. Br J Sports Med 2016;50:1030–1041. doi:10.1136/bjsports-2016-096581







Leave a Reply
Want to join the discussion?Feel free to contribute!