 PATELLAR INSTABILITY
PATELLAR INSTABILITY
Patellofemoral joint instability is one of the most common knee problems seen in the adolescent population. A primary (first-time) patellar dislocation occurs in 23 to 42 per 100,000 people per year, often leading to pain, a variety of functional impairments, and further dislocations.1 Stability of the knee joint is dependent on both bony and soft tissue restraints. The etiology of the disorder is multifactorial and often related to structural compromise or an imbalance of such restraints.2 3 4 72% of initial dislocations are sustained during a sporting event, especially in those that require cutting and pivoting, such as soccer, basketball, and football. 5 6
Anatomy and Alignment of the Knee
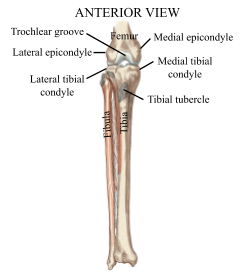 The knee joint is the largest joint in the body and has a high functional demand. Mobility is provided by the bony structures of the joint while stability is provided by the surrounding soft tissues, making it very susceptible to injury. It consists of three bones that play a direct role in the knee joint, including the femur (thigh bone), tibia (shin bone), and patella (knee cap). The fibula, which is the smaller shin bone that runs along the outside of the tibia, has no direct function at the joint, but provides a key attachment point for important muscles and ligaments. 7
The knee joint is the largest joint in the body and has a high functional demand. Mobility is provided by the bony structures of the joint while stability is provided by the surrounding soft tissues, making it very susceptible to injury. It consists of three bones that play a direct role in the knee joint, including the femur (thigh bone), tibia (shin bone), and patella (knee cap). The fibula, which is the smaller shin bone that runs along the outside of the tibia, has no direct function at the joint, but provides a key attachment point for important muscles and ligaments. 7
Femur
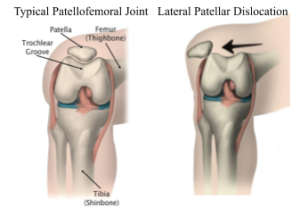
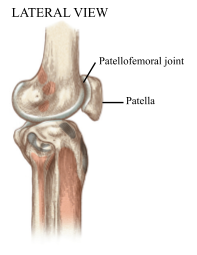
The distal (bottom) end of the femur is shaped similar to a knuckle, with large bumps on either side termed lateral and medial condyles. Lateral and medial epicondyles project from their respective 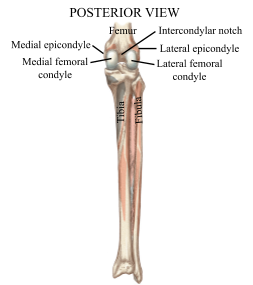 condyles, which are used as attachment sites for important ligaments. On the posterior (back) side of the femur, the condyles are separated by a deep passage called the intercondylar notch, which creates a tunnel for ligamentous structures. The femoral condyles join together anteriorly to create the trochlear (intercondylar) groove, which articulates with the patella, forming the patellofemoral joint.8
condyles, which are used as attachment sites for important ligaments. On the posterior (back) side of the femur, the condyles are separated by a deep passage called the intercondylar notch, which creates a tunnel for ligamentous structures. The femoral condyles join together anteriorly to create the trochlear (intercondylar) groove, which articulates with the patella, forming the patellofemoral joint.8
 Tibia and Fibula
Tibia and Fibula
As stated earlier, the fibula does not play a direct function at the knee joint, however it provides an attachment point for key muscles and ligaments that support the knee. The tibia is the primary weightbearing shin bone, meaning it is the main structure that accepts the weight of the body. The proximal (top) end of the tibia flares into lateral and medial condyles, which forms a broad region referred to as the tibial plateau. The tibial plateau accepts the condyles of the femur, creating the compartments of the tibiofemoral joint. On the anterior (front) aspect of the proximal tibia is the tibial tubercle, a bony prominence that serves as the distal attachment point of the quadriceps (thigh) muscle via the patellar tendon.9
Patella
The patella is the largest sesamoid (“floating”) bone in the body. It lies within the intercondylar groove of the femur, providing a point of attachment for both the quadriceps tendon and the patellar tendon. The primary purpose of the patella is to increase the leverage of the quadriceps by increasing the moment arm of the patellar tendon. Additionally, the patella helps protect the quadriceps tendon from frictional 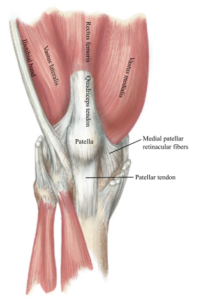 forces, and acts as a shield for deeper structures of the knee joint. The posterior aspect of the patella articulates with the trochlear groove of the femur, creating the patellofemoral joint.10
forces, and acts as a shield for deeper structures of the knee joint. The posterior aspect of the patella articulates with the trochlear groove of the femur, creating the patellofemoral joint.10
Medial Patellofemoral Ligament
Ligaments are bands of fibrous tissue that attach bone to bone. The ligaments of the knee that are most often spoken about include the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL). These ligaments help prevent excessive knee motion and provide dynamic stability to the joint. However, one important ligament that is often overlooked is the medial patellofemoral ligament (MPFL). This broad, thin ligament flows down from the medial (inside) border of the patella and interconnects the patella, femur, tibia, and other structures, and is considered the main passive stabilizer of the patellofemoral joint.11 This structure is most important during the first 30 degrees of knee flexion (bend), where it experiences maximal load from the quadriceps muscle and provides 60% of the resistance to lateral (outward) patellar movement.12 The primary function of the MPFL is to guide the patella into the trochlear groove in early flexion, where the bony restraints of the trochlea contribute less to the stability of the patella. During deeper ranges of knee flexion, the role of the MPFL is decreased and the patella receives its stability from the trochlea.13 14
Types
Traumatic (Acute) Instability
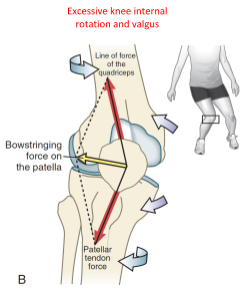 Patellar dislocation occurs when the patella has been disengaged from the trochlear groove. This typically occurs in the lateral direction due to the overall lateral line of force the quadriceps relative to the patella.15 16 Acute traumatic patellar dislocations account for approximately 3% of all knee injuries, while 50-60% of first-time lateral patellar dislocations being sports-related.1718 Many of these injuries occur as a result of a non-contact injury. The most common mechanism of injury results from the knee being placed in a position of flexion and internal rotation on a planted foot with a valgus (inward) component.19 20 2122 It is possible for patellar dislocations to occur as a result of a contact injury or direct blow to the knee. With this mechanism of injury, the underlying patellofemoral joint anatomy is usually normal.23 This can lead to damage or rupture of the medial soft tissues that are responsible for stabilizing the patella, specifically the MPFL. Traumatic dislocations increase the risk of subsequent recurrence, which has been reported to be as high as 25-45%.24
Patellar dislocation occurs when the patella has been disengaged from the trochlear groove. This typically occurs in the lateral direction due to the overall lateral line of force the quadriceps relative to the patella.15 16 Acute traumatic patellar dislocations account for approximately 3% of all knee injuries, while 50-60% of first-time lateral patellar dislocations being sports-related.1718 Many of these injuries occur as a result of a non-contact injury. The most common mechanism of injury results from the knee being placed in a position of flexion and internal rotation on a planted foot with a valgus (inward) component.19 20 2122 It is possible for patellar dislocations to occur as a result of a contact injury or direct blow to the knee. With this mechanism of injury, the underlying patellofemoral joint anatomy is usually normal.23 This can lead to damage or rupture of the medial soft tissues that are responsible for stabilizing the patella, specifically the MPFL. Traumatic dislocations increase the risk of subsequent recurrence, which has been reported to be as high as 25-45%.24
Atraumatic (Chronic) Instability
In chronic instability, the patella typically only slides partially out of the groove before returning to its natural pathway, which is known as a subluxation. It is not uncommon for this type of instability to be described with vague complaints that may not identify a discrete event of patellar dislocation. Common complaints may include the knee “giving out” with jumping or pivoting activities, unexpected instability with simple daily tasks, and anterior knee pain. 25Compared to traumatic instability, chronic instability is mostly associated with anomalies of the patellofemoral joint, which will be describe in the following section. 26 Individuals with a history of patellar instability are seven times more likely to experience subsequent instability episodes versus first-time dislocators.27
Predisposing Factors
Factors that contribute to patellar instability are often multifactorial and cannot be attributed to a single cause. The anatomy of each individual is often not straight forward, and deciding a treatment plan may pose as a challenge. 28
Anatomic Factors
Patella alta
 Often referred to as a “high-riding kneecap”, patella alta describes an increased height of the patella in relation to the femoral groove, where the groove is very shallow. This requires higher degrees of knee flexion in order for the patella to engage in the trochlear groove, resulting in decreased bony stability provided by the bony structure. The patella is required to travel a longer distance outside of the confines of the trochlear groove, ultimately increasing the likelihood of lateral dislocation in the early arc of knee motion.2930 31 Patellar height is measured using common indices including Insall-Salvati (IS) and Caton-Deschamps index (CDI) from lateral radiographs. It is worth noting that patellar height is often greater in pediatric patients, which should be taken into consideration when using the cut-off values from the measurement indices. Patella alta has been reported to be present in 50% of individuals with acute patellar instability. Individuals who experienced dislocations with minimal trauma are more likely to have an increased patellar height compared to those with traumatic dislocations, and are much more likely to sustain recurrent dislocations following conservative treatment.32 The odds of recurrent instability due to patella alta was reported to be as high as 10.6 times greater compared to those without. 33 A meta-analysis has shown patella alta to be a significant risk factor for recurrence.1 However, patella alta rarely occurs in isolation with patellar instability.34 It is often associated with trochlear dysplasia, and is most valuable as a risk factor when combined with other factors, such as trochlear dysplasia and increased tibial tubercle-trochlear groove distance, which will both be described next in this section.35 36
Often referred to as a “high-riding kneecap”, patella alta describes an increased height of the patella in relation to the femoral groove, where the groove is very shallow. This requires higher degrees of knee flexion in order for the patella to engage in the trochlear groove, resulting in decreased bony stability provided by the bony structure. The patella is required to travel a longer distance outside of the confines of the trochlear groove, ultimately increasing the likelihood of lateral dislocation in the early arc of knee motion.2930 31 Patellar height is measured using common indices including Insall-Salvati (IS) and Caton-Deschamps index (CDI) from lateral radiographs. It is worth noting that patellar height is often greater in pediatric patients, which should be taken into consideration when using the cut-off values from the measurement indices. Patella alta has been reported to be present in 50% of individuals with acute patellar instability. Individuals who experienced dislocations with minimal trauma are more likely to have an increased patellar height compared to those with traumatic dislocations, and are much more likely to sustain recurrent dislocations following conservative treatment.32 The odds of recurrent instability due to patella alta was reported to be as high as 10.6 times greater compared to those without. 33 A meta-analysis has shown patella alta to be a significant risk factor for recurrence.1 However, patella alta rarely occurs in isolation with patellar instability.34 It is often associated with trochlear dysplasia, and is most valuable as a risk factor when combined with other factors, such as trochlear dysplasia and increased tibial tubercle-trochlear groove distance, which will both be described next in this section.35 36
Trochlear dysplasia
 Trochlear dysplasia is described as the flattening or alteration of the joint surface of the trochlea with a less pronounced concavity of the groove. When the trochlear groove is deficient, it is unable to offer the bony constraints that are required in order to stabilize the patella as the knee begins to flex, forcing the MPFL to take on a greater role. 3738 Trochlear dysplasia has been classified into four types: Type A-D, each being identified by specific characteristics on lateral radiographs.39 This results in a considerable loss of lateral patellar tracking, ultimately leading to instability and an increased likelihood of a lateral patellar dislocation.40 41
Trochlear dysplasia is described as the flattening or alteration of the joint surface of the trochlea with a less pronounced concavity of the groove. When the trochlear groove is deficient, it is unable to offer the bony constraints that are required in order to stabilize the patella as the knee begins to flex, forcing the MPFL to take on a greater role. 3738 Trochlear dysplasia has been classified into four types: Type A-D, each being identified by specific characteristics on lateral radiographs.39 This results in a considerable loss of lateral patellar tracking, ultimately leading to instability and an increased likelihood of a lateral patellar dislocation.40 41 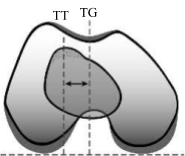 It has been reported that 66-96% of patients who have experienced an instability event demonstrate radiographic evidence of a dysplastic trochlea. 42
It has been reported that 66-96% of patients who have experienced an instability event demonstrate radiographic evidence of a dysplastic trochlea. 42
43 44Additionally, the presence of trochlear dysplasia, regardless of severity, was significantly associated with an increased risk of recurrence. 45 This anatomic anomaly is considered a major factor that has been consistently identified in patients with lateral patellar dislocations and is one of the strongest predictors for recurrent stability, even if it is present in isolation. As previously stated, trochlear dysplasia is often associated with patella alta, and when found in combination there is an increased risk of dislocation by 41-fold. 4647 48 If a lateral patellar dislocation occurs during low-risk or no-risk pivoting activities, such as walking, cycling, or running, it is likely related to trochlear dysplasia. 49
Tibial Tubercle-Trochlear Groove Distance
 The distance between the midpoint of the tibial tubercle and the deepest point of the trochlear groove in the transverse plane (birds-eye view) is referred to as the tibial tubercle-trochlear groove (TT-TG) distance.50 Magnetic resonance imaging (MRI) is used to calculate this distance, which quantifies the quadriceps vector and is used to measure malalignment in relation to the patellar tendon. 51 In a typical knee joint, the tibial tubercle lies relatively vertical underneath the femoral sulcus, which directs the force vector of the quadriceps muscle inferiorly during knee flexion. A TT-TG distance <15 mm is considered normal, while 15-20 mm is considered borderline, and anything >20 mm is defined as excessive. A TT-TG distance of >20 mm is almost always associated with patellar instability and is significantly associated with an increased risk of recurrence, increasing the odds of rediclocation by 2.9 times versus individuals with a normal TT-TG distance.5253 54 Studies have demonstrated a significantly greater TT-TG distance in children with patellar instability when compared to those without evidence of instability.55 Additionally, if there is an excessively lateral distance of the tibial tubercle relative to the trochlear groove, this predisposes patients to lateral maltracking of the patella and therefore increasing the risk for an instability event to occur.56
The distance between the midpoint of the tibial tubercle and the deepest point of the trochlear groove in the transverse plane (birds-eye view) is referred to as the tibial tubercle-trochlear groove (TT-TG) distance.50 Magnetic resonance imaging (MRI) is used to calculate this distance, which quantifies the quadriceps vector and is used to measure malalignment in relation to the patellar tendon. 51 In a typical knee joint, the tibial tubercle lies relatively vertical underneath the femoral sulcus, which directs the force vector of the quadriceps muscle inferiorly during knee flexion. A TT-TG distance <15 mm is considered normal, while 15-20 mm is considered borderline, and anything >20 mm is defined as excessive. A TT-TG distance of >20 mm is almost always associated with patellar instability and is significantly associated with an increased risk of recurrence, increasing the odds of rediclocation by 2.9 times versus individuals with a normal TT-TG distance.5253 54 Studies have demonstrated a significantly greater TT-TG distance in children with patellar instability when compared to those without evidence of instability.55 Additionally, if there is an excessively lateral distance of the tibial tubercle relative to the trochlear groove, this predisposes patients to lateral maltracking of the patella and therefore increasing the risk for an instability event to occur.56
Q angle
The magnitude and direction of force produced by the quadriceps have an 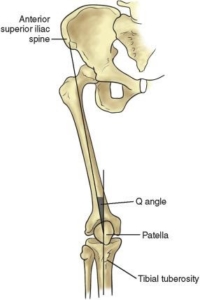 important influence on the biomechanics of the patellofemoral joint. The overall line of pull of the muscle relative to the patella is termed as the Q angle, which provides a quick method for physical therapists to grossly assess the angle of pull on the patella. This angle is formed by creating vectors between the bony prominence at the top of the hip, termed the anterior superior iliac spine (ASIS), and the midpoint of the patella, and another connecting the midpoint of the patella to the tibial tubercle. The American Orthopedic Association defines normal values as 10-15 degrees, with men generally having smaller measurements and women being on the higher end. A Q angle of >20 degrees indicates significant malalignment. Similar to the anatomic anomalies previously mentioned, an increased Q angle places a larger lateral force is placed on the patella, ultimately increasing the risk of patellar instability and likelihood of dislocation. 57 58
important influence on the biomechanics of the patellofemoral joint. The overall line of pull of the muscle relative to the patella is termed as the Q angle, which provides a quick method for physical therapists to grossly assess the angle of pull on the patella. This angle is formed by creating vectors between the bony prominence at the top of the hip, termed the anterior superior iliac spine (ASIS), and the midpoint of the patella, and another connecting the midpoint of the patella to the tibial tubercle. The American Orthopedic Association defines normal values as 10-15 degrees, with men generally having smaller measurements and women being on the higher end. A Q angle of >20 degrees indicates significant malalignment. Similar to the anatomic anomalies previously mentioned, an increased Q angle places a larger lateral force is placed on the patella, ultimately increasing the risk of patellar instability and likelihood of dislocation. 57 58
Ligamentous laxity
 A secondary factor that may contribute to patellar instability includes generalized ligamentous laxity. This results in an increased range of motion of various joints compared to the average range of motion in the general population, termed joint hypermobility.5960
A secondary factor that may contribute to patellar instability includes generalized ligamentous laxity. This results in an increased range of motion of various joints compared to the average range of motion in the general population, termed joint hypermobility.5960
It has been estimated between 5% and 15% of the general population demonstrate hypermobility. It is most commonly seen in children and adolescents and is slightly more prevalent in women.61 62 Joint hypermobility may exist in isolation, however it may also be a result of various connective tissue disorders, such as Ehlers-Danlos syndrome or Marfan syndrome. 63 6465
There are a number of clinical scoring systems for measuring joint laxity, a common one being the Beighton score. It involves a set of five maneuvers used to judge if an individual demonstrates evidence of hypermobility. Although there is no universal cut off score, receiving a score of 4 or more out of 9 is typically used to indicate generalized hypermobility. Findings suggest individuals with general ligamentous laxity may have higher risk of suffering from musculoskeletal injuries, which include patellar dislocations. 66 Because there is minimal active control of valgus loads at the knee joint, stability relies almost completely on passive stabilizers to prevent injury. In turn, when a valgus forces is applied to the knee while the foot remains planted, a greater internal torque is placed on a lax MPFL, which further predisposes it to injury. 67
Management Options
Nonoperative
Rehabilitation
Immediate surgical intervention is rarely indicated after a patellar dislocation, and conservative treatment is often recommended after a first-time traumatic dislocation if there is no evidence of severe injury to the bone or soft tissue. Currently, there is no consensus on a post-injury protocol, and management and progression may vary based on the provider. Initial management should focus on controlling pain and swelling, protecting the knee from further injury, and early range of motion.6869 70 This is achieved by the use of modalities (e.g. ice) and a hinged knee brace with axillary crutches. Individuals are typically allowed to bear as much weight on the affected extremity as tolerable with the brace locked in full extension or 20 degrees of knee flexion, as this position places the least amount of strain on the MPFL. Once acute inflammation has subsided, early physical therapy is often recommended in order to progressively regain full range of motion of the knee, improve muscle strength and balance, and normalizing gait patterns.71 727374 There is no specified timeframe for rehabilitation after a patellar dislocation. Extensive physical therapy is likely indicated in order to recover normalcy of motion, strength, dynamic stability of the involved limb, and to increase the confidence in their knee. Studies have shown 75% of patients reported good or excellent results following nonoperative management, however, the rate of recurrent instability events have been reported to range from 35-50%. 7576 7778
Operative
Surgical indications
Non-operative treatment is typically attempted for about 3-6 months after a primary patellar instability event. 79 80 81 If this fails, surgical intervention is then considered. The primary indications for surgical intervention after a first-time patellar dislocation include the presence of a large osteochondral fragment, femoral avulsion injury of the medial stabilizers, or significant malalignment or trochlear dysplasia. 82 838485 A combination of pre-operative imaging and a thorough understanding of the etiology of instability must be used to determine whether or not conservative management is appropriate. Imaging studies provide an insight to any bony pathology of the patellofemoral joint, and can help guide surgeons on the most appropriate surgical procedure to perform if indicated.8687 However, there other situations that surgical intervention may be warranted, even in the absence of an such indications. A significant factor that may endorse surgical management is the loss of confidence in the affected knee and loss of function that compromises the individual’s level of activity or daily life function.88
The goal of surgery is to restore the restraining function of medial stabilizers and reestablish the primary restraint to lateral translation of the patella. 89 90 Surgical procedures for patellar instability can be divided into two categories, including proximal and distal realignment. Proximal realignment is typically performed on the soft tissue stabilizers of the knee, which includes MPFL reconstruction. Distal realignment refers to the change in position of the tibial tubercle, which can be achieved by several different osteotomy techniques. 9192 The most common method for managing lateral patellar instability is reconstruction of the MPFL. The grafts used to reconstruct the MPFL are typically either autografts or allografts of various tendons. An autograft is tissue that is harvested from the patient undergoing the operation, whereas an allograft is tissue obtained by a human donor. Common grafts used with MPFL reconstruction include gracilis tendon and semitendinosus tendon.939495 There is limited research that compares patient outcomes based on the graft type with MPFL reconstruction. Recent studies have compared whether the type of graft affects the rate of recurrent instability after surgery. Results demonstrated an overall low rate of recurrence of 2% for both autografts and allografts, with no significant difference found between the graft types and no significant difference in clinical outcomes with semitendinosus and gracilis autografts. This differs from the common ACL reconstruction, where autograft has been shown to be the superior option. 9697 With chronic patellar instability, it is unlikely to obtain good outcomes with an isolated MPFL reconstruction. Correction of the underlying anatomic factors contributing to instability should be addressed in addition to MPFL reconstruction in order to achieve proper balance of medial and lateral forces on the patellofemoral joint.98 This is achieved by using a combination of proximal and distal procedures.99100 Overall, excellent outcomes have been demonstrated following MPFL reconstruction in terms of recurrent instability and function.18 Redislocation rates have been reported to be as low, with recurrence rates being lower in adults when compared to adolescents, ranging from 1.2% to 4% for adults and 10% to 24% for pediatric and adolescents.101102 Another study reported good or excellent functional outcomes with MPFL reconstruction in 95% of patients.103
Post-Operative Rehabilitation
Post-operative rehabilitation is extensive and often requires months of physical therapy in order to ensure full recovery and normal function of the impaired extremity. The rehabilitation timeline is typically broken down into different phases:
Early Phase
Range of motion and ambulation (walking) is progressed as tolerated immediately after surgery, as immobilization of the knee can result in stiffness and loss of motion.104 Individuals are allowed to bear weight through the operated extremity to tolerance immediately. Crutches are typically used while wearing a hinged knee brace that is locked in full knee extension with all activity (except when sitting or at rest) in order to facilitate a normal heel-toe pattern with walking. Once a normal gait pattern is achieved, individuals can gradually wean off crutches while maintaining this normal pattern to prevent any abnormal gait deviations. This is typically initiated 2-4 weeks after surgery. 105
Regaining muscle control of the quadriceps is an important part of the early phase of rehabilitation. Pain and swelling are known contributors to the inhibition of quadriceps recruitment post-operatively, so it is important to use modalities in order to manage these factors. Applying ice often is an easy method to relieve pain and control swelling. Neuromuscular electrical stimulation (NMES) has been shown to reduce the strength loss in the knee after ligamentous surgery if quadriceps inhibition is demonstrated. NMES involves “reteaching” the muscle how to contract properly again following surgery. An electrical current is sent through the muscle, causing the muscle to contract as if the individual were contracting it themselves. Volitional contraction is typically performed with the NMES to maximize muscle recruitment.
Common exercises during the early phase include quadricep sets (“quad sets”), heel slides, straight leg raises, and weight shifting drills. Mini squats and light general leg strengthening can be added as tolerated in order to improve control of the knee with dynamic movements. Clinical milestones that indicate safe progression to the next phase includes normal gait with brace and assistive device, 90 degrees of knee range of motion, and no increase in swelling.106
Intermediate Phase
The primary goals of this phase of physical therapy include gradual restoration of full knee range of motion, gradual progression of strengthening exercises, and maintaining a normal gait pattern. At this point in rehabilitation, knee range of motion should be well established. If not, more aggressive techniques may be utilized in order to achieve motion equal to that of the unaffected extremity.
Strengthening can be progressed by adding weight or by challenging the balance component with exercise, such as squatting on a piece of foam. Additional closed chain exercises (feet on the ground) can be initiated, including lunges, leg press, and glute bridges. Single-leg exercise can be initiated in the latter half of the phase to address potential compensations to address both balance and dynamic control of the knee.
Balance is a very important, often forgotten about, piece of rehabilitation that translates to the dynamic stability and control of the lower extremity, especially with squatting, pivoting, and cutting activities. Clinical milestones that indicate progression to the next phase include the ability to stand on one leg, full range of motion, and demonstration of good quadriceps control with exercises.107
Late Phase
The primary goal of the final phase of rehabilitation is to obtain lower extremity strength of at least 80-90% of the unaffected leg, and to progressively reintroduce functional and sporting activities. It is important to gradually increase the forces applied to the joint to ensure the graft and surrounding tissue is able to adapt after a prolonged period of decreased loading relative to the prior level of function.
Higher level plyometric activities can be initiated by including double leg jumping in place. Progression of jumping and/or hopping should always begin bilateral (both legs) progressing to unilateral (single leg). Light jogging is initiated at 3-4 months after surgery.108109 110
Return to Sport Testing
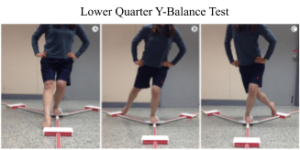 Time until resuming preinjury sport and activity is often the primary concern after surgery. In the past, return to sport (RTS) clearance was solely based on the amount of time after surgery. Currently, efforts have been made to shift away from this time-based RTS criteria and more towards guidelines that are based on functional performance. Full RTS clearance is often based on successful rehabilitation, which can be evaluated using a battery of tests consisting of a number of measures and functional activities. Prerequisites for allowing RTS typically include the absence of pain and swelling, full range of motion, quadriceps strength of at least 90% of the uninjured leg, and no sensation of instability or evidence of compensations with
Time until resuming preinjury sport and activity is often the primary concern after surgery. In the past, return to sport (RTS) clearance was solely based on the amount of time after surgery. Currently, efforts have been made to shift away from this time-based RTS criteria and more towards guidelines that are based on functional performance. Full RTS clearance is often based on successful rehabilitation, which can be evaluated using a battery of tests consisting of a number of measures and functional activities. Prerequisites for allowing RTS typically include the absence of pain and swelling, full range of motion, quadriceps strength of at least 90% of the uninjured leg, and no sensation of instability or evidence of compensations with 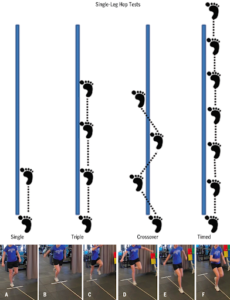 cutting or pivoting drills.111112 Recovery of quadriceps strength can be assessed by measuring the amount of force it is capable of producing at 90 degrees of knee flexion, while dynamic knee stability can be assessed by using functional performance tests (FPT), such as a the Lower Quarter Y-Balance Test, a single-leg hop, and a cross over hop test. A recent study compared the results of the measured strength of the quadriceps and RTS testing between surgical limb and uninvolved limb. At an average of 7.5 months after surgery, 56% of patients demonstrated inadequate quadriceps strength, while 68% were unable to adequately perform the hop tests that were administered. Although rehabilitation timelines tend to vary based on the surgeon and the given protocol, it has been demonstrated that adolescent athletes may require prolonged rehabilitation programs that go beyond 8 months in order to allow recovery of normal muscle strength and dynamic stability for safe RTS, and the previous time-based criteria for RTS is likely inadequate. It has been shown that individuals that achieve 90% of strength and dynamic performance relative to the unaffected limb demonstrate a similar performance in activity compared to uninjured persons.113
cutting or pivoting drills.111112 Recovery of quadriceps strength can be assessed by measuring the amount of force it is capable of producing at 90 degrees of knee flexion, while dynamic knee stability can be assessed by using functional performance tests (FPT), such as a the Lower Quarter Y-Balance Test, a single-leg hop, and a cross over hop test. A recent study compared the results of the measured strength of the quadriceps and RTS testing between surgical limb and uninvolved limb. At an average of 7.5 months after surgery, 56% of patients demonstrated inadequate quadriceps strength, while 68% were unable to adequately perform the hop tests that were administered. Although rehabilitation timelines tend to vary based on the surgeon and the given protocol, it has been demonstrated that adolescent athletes may require prolonged rehabilitation programs that go beyond 8 months in order to allow recovery of normal muscle strength and dynamic stability for safe RTS, and the previous time-based criteria for RTS is likely inadequate. It has been shown that individuals that achieve 90% of strength and dynamic performance relative to the unaffected limb demonstrate a similar performance in activity compared to uninjured persons.113
Conclusion
Patellar instability is a common injury seen mostly in the athletic adolescent population. Contributing factors are likely multifactorial, and the etiology of the injury must be understood in order to determine appropriate management. Regardless of the management choice, whether operative or nonoperative, physical therapy is an important piece of recovery in order to help individuals recover adequate muscle strength, improve dynamic control of the affected lower extremity, and regain confidence in the affected knee with high-level activities.
- Huntington LS, Webster KE, Devitt BM, Scanlon JP, Feller JA. Factors Associated With an Increased Risk of Recurrence After a First-Time Patellar Dislocation: A Systematic Review and Meta-analysis. Am J Sports Med. December 2019:036354651988846. doi:10.1177/0363546519888467
- DeFroda SF, Gil JA, Boulos A, Cruz AI. Diagnosis and Management of Traumatic Patellar Instability in the Pediatric Patient. Orthopedics. 2017;40(5):e749-e757. doi:10.3928/01477447-20170602-04
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Sanchis-Alfonso V. How to Deal With Chronic Patellar Instability: What Does the Literature Tell Us? Sports Health Multidiscip Approach. 2016;8(1):86-90. doi:10.1177/1941738115604156
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C. Characteristics of Patients with Primary Acute Lateral Patellar Dislocation and Their Recovery within the First 6 Months of Injury. Am J Sports Med. 2000;28(4):472-479. doi:10.1177/03635465000280040601
- Neumann DA, Kelly ER, Kiefer CL, Martens K, Grosz CM. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation.; 2017.
- Neumann DA, Kelly ER, Kiefer CL, Martens K, Grosz CM. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation.; 2017.
- Neumann DA, Kelly ER, Kiefer CL, Martens K, Grosz CM. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation.; 2017.
- Neumann DA, Kelly ER, Kiefer CL, Martens K, Grosz CM. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation.; 2017.
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Neumann DA, Kelly ER, Kiefer CL, Martens K, Grosz CM. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation.; 2017.
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Fisher B, Nyland J, Brand E, Curtin B. Medial Patellofemoral Ligament Reconstruction for Recurrent Patellar Dislocation: A Systematic Review Including Rehabilitation and Return-to-Sports Efficacy. Arthrosc J Arthrosc Relat Surg. 2010;26(10):1384-1394. doi:10.1016/j.arthro.2010.04.005
- Neumann DA, Kelly ER, Kiefer CL, Martens K, Grosz CM. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation.; 2017.
- Diederichs G, Issever AS, Scheffler S. MR Imaging of Patellar Instability: Injury Patterns and Assessment of Risk Factors . RadioGraphics. 2010;30(4):961-981. doi:10.1148/rg.304095755
- DeFroda SF, Gil JA, Boulos A, Cruz AI. Diagnosis and Management of Traumatic Patellar Instability in the Pediatric Patient. Orthopedics. 2017;40(5):e749-e757. doi:10.3928/01477447-20170602-04
- Parikh SN, Lykissas MG, Gkiatas I. Predicting Risk of Recurrent Patellar Dislocation. Curr Rev Musculoskelet Med. 2018;11(2):253-260. doi:10.1007/s12178-018-9480-5
- DeFroda SF, Gil JA, Boulos A, Cruz AI. Diagnosis and Management of Traumatic Patellar Instability in the Pediatric Patient. Orthopedics. 2017;40(5):e749-e757. doi:10.3928/01477447-20170602-04
- Diederichs G, Issever AS, Scheffler S. MR Imaging of Patellar Instability: Injury Patterns and Assessment of Risk Factors . RadioGraphics. 2010;30(4):961-981. doi:10.1148/rg.304095755
- Parikh SN, Lykissas MG, Gkiatas I. Predicting Risk of Recurrent Patellar Dislocation. Curr Rev Musculoskelet Med. 2018;11(2):253-260. doi:10.1007/s12178-018-9480-5
- Diduch DR, Kandil A, Burrus MT. Lateral Patellar Instability in the Skeletally Mature Patient: Evaluation and Surgical Management. J Am Acad Orthop Surg. 2018;26(12):429-439. doi:10.5435/JAAOS-D-16-00052
- Parikh SN, Lykissas MG, Gkiatas I. Predicting Risk of Recurrent Patellar Dislocation. Curr Rev Musculoskelet Med. 2018;11(2):253-260. doi:10.1007/s12178-018-9480-5
- DeFroda SF, Gil JA, Boulos A, Cruz AI. Diagnosis and Management of Traumatic Patellar Instability in the Pediatric Patient. Orthopedics. 2017;40(5):e749-e757. doi:10.3928/01477447-20170602-04
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Parikh SN, Lykissas MG, Gkiatas I. Predicting Risk of Recurrent Patellar Dislocation. Curr Rev Musculoskelet Med. 2018;11(2):253-260. doi:10.1007/s12178-018-9480-5
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Diduch DR, Kandil A, Burrus MT. Lateral Patellar Instability in the Skeletally Mature Patient: Evaluation and Surgical Management. J Am Acad Orthop Surg. 2018;26(12):429-439. doi:10.5435/JAAOS-D-16-00052
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Diederichs G, Issever AS, Scheffler S. MR Imaging of Patellar Instability: Injury Patterns and Assessment of Risk Factors <sup/>. RadioGraphics. 2010;30(4):961-981. doi:10.1148/rg.304095755
- Diduch DR, Kandil A, Burrus MT. Lateral Patellar Instability in the Skeletally Mature Patient: Evaluation and Surgical Management. J Am Acad Orthop Surg. 2018;26(12):429-439. doi:10.5435/JAAOS-D-16-00052
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Parikh SN, Lykissas MG, Gkiatas I. Predicting Risk of Recurrent Patellar Dislocation. Curr Rev Musculoskelet Med. 2018;11(2):253-260. doi:10.1007/s12178-018-9480-5
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- DeFroda SF, Gil JA, Boulos A, Cruz AI. Diagnosis and Management of Traumatic Patellar Instability in the Pediatric Patient. Orthopedics. 2017;40(5):e749-e757. doi:10.3928/01477447-20170602-04
- Parikh SN, Lykissas MG, Gkiatas I. Predicting Risk of Recurrent Patellar Dislocation. Curr Rev Musculoskelet Med. 2018;11(2):253-260. doi:10.1007/s12178-018-9480-5
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Parikh SN, Lykissas MG, Gkiatas I. Predicting Risk of Recurrent Patellar Dislocation. Curr Rev Musculoskelet Med. 2018;11(2):253-260. doi:10.1007/s12178-018-9480-5
- Batailler C, Neyret P. Trochlear dysplasia: imaging and treatment options. EFORT Open Rev. 2018;3(5):240-247. doi:10.1302/2058-5241.3.170058
- DeFroda SF, Gil JA, Boulos A, Cruz AI. Diagnosis and Management of Traumatic Patellar Instability in the Pediatric Patient. Orthopedics. 2017;40(5):e749-e757. doi:10.3928/01477447-20170602-04
- Diederichs G, Issever AS, Scheffler S. MR Imaging of Patellar Instability: Injury Patterns and Assessment of Risk Factors <sup/>. RadioGraphics. 2010;30(4):961-981. doi:10.1148/rg.304095755
- DeFroda SF, Gil JA, Boulos A, Cruz AI. Diagnosis and Management of Traumatic Patellar Instability in the Pediatric Patient. Orthopedics. 2017;40(5):e749-e757. doi:10.3928/01477447-20170602-04
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Parikh SN, Lykissas MG, Gkiatas I. Predicting Risk of Recurrent Patellar Dislocation. Curr Rev Musculoskelet Med. 2018;11(2):253-260. doi:10.1007/s12178-018-9480-5
- Huntington LS, Webster KE, Devitt BM, Scanlon JP, Feller JA. Factors Associated With an Increased Risk of Recurrence After a First-Time Patellar Dislocation: A Systematic Review and Meta-analysis. Am J Sports Med. December 2019:036354651988846. doi:10.1177/0363546519888467
- DeFroda SF, Gil JA, Boulos A, Cruz AI. Diagnosis and Management of Traumatic Patellar Instability in the Pediatric Patient. Orthopedics. 2017;40(5):e749-e757. doi:10.3928/01477447-20170602-04
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Parikh SN, Lykissas MG, Gkiatas I. Predicting Risk of Recurrent Patellar Dislocation. Curr Rev Musculoskelet Med. 2018;11(2):253-260. doi:10.1007/s12178-018-9480-5
- Parikh SN, Lykissas MG, Gkiatas I. Predicting Risk of Recurrent Patellar Dislocation. Curr Rev Musculoskelet Med. 2018;11(2):253-260. doi:10.1007/s12178-018-9480-5
- Pandit S, Frampton C, Stoddart J, Lynskey T. Magnetic resonance imaging assessment of tibial tuberosity–trochlear groove distance: normal values for males and females. Int Orthop. 2011;35(12):1799-1803. doi:10.1007/s00264-011-1240-8
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Huntington LS, Webster KE, Devitt BM, Scanlon JP, Feller JA. Factors Associated With an Increased Risk of Recurrence After a First-Time Patellar Dislocation: A Systematic Review and Meta-analysis. Am J Sports Med. December 2019:036354651988846. doi:10.1177/0363546519888467
- Diederichs G, Issever AS, Scheffler S. MR Imaging of Patellar Instability: Injury Patterns and Assessment of Risk Factors <sup/>. RadioGraphics. 2010;30(4):961-981. doi:10.1148/rg.304095755
- Carlson VR, Boden BP, Shen A, Jackson JN, Yao L, Sheehan FT. The Tibial Tubercle-Trochlear Groove Distance Is Greater in Patients With Patellofemoral Pain: Implications for the Origin of Pain and Clinical Interventions. Am J Sports Med. 2017;45(5):1110-1116. doi:10.1177/0363546516681002
- Pennock AT, Alam M, Bastrom T. Variation in Tibial Tubercle–Trochlear Groove Measurement as a Function of Age, Sex, Size, and Patellar Instability. Am J Sports Med. 2014;42(2):389-393. doi:10.1177/0363546513509058
- Carlson VR, Boden BP, Shen A, Jackson JN, Yao L, Sheehan FT. The Tibial Tubercle-Trochlear Groove Distance Is Greater in Patients With Patellofemoral Pain: Implications for the Origin of Pain and Clinical Interventions. Am J Sports Med. 2017;45(5):1110-1116. doi:10.1177/0363546516681002
- DeFroda SF, Gil JA, Boulos A, Cruz AI. Diagnosis and Management of Traumatic Patellar Instability in the Pediatric Patient. Orthopedics. 2017;40(5):e749-e757. doi:10.3928/01477447-20170602-04
- Neumann DA, Kelly ER, Kiefer CL, Martens K, Grosz CM. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation.; 2017.
- Bin Abd Razak HR, Bin Ali N, Howe TS. Generalized ligamentous laxity may be a predisposing factor for musculoskeletal injuries. J Sci Med Sport. 2014;17(5):474-478. doi:10.1016/j.jsams.2013.11.001
- Pacey V, Nicholson LL, Adams RD, Munn J, Munns CF. Generalized Joint Hypermobility and Risk of Lower Limb Joint Injury During Sport: A Systematic Review With Meta-Analysis. Am J Sports Med. 2010;38(7):1487-1497. doi:10.1177/0363546510364838
- Bin Abd Razak HR, Bin Ali N, Howe TS. Generalized ligamentous laxity may be a predisposing factor for musculoskeletal injuries. J Sci Med Sport. 2014;17(5):474-478. doi:10.1016/j.jsams.2013.11.001
- Remvig L, Jensen DV, Ward RC. Epidemiology of general joint hypermobility and basis for the proposed criteria for benign joint hypermobility syndrome: review of the literature. J Rheumatol. 2007;34(4):804-809.
- DeFroda SF, Gil JA, Boulos A, Cruz AI. Diagnosis and Management of Traumatic Patellar Instability in the Pediatric Patient. Orthopedics. 2017;40(5):e749-e757. doi:10.3928/01477447-20170602-04
- Diederichs G, Issever AS, Scheffler S. MR Imaging of Patellar Instability: Injury Patterns and Assessment of Risk Factors <sup/>. RadioGraphics. 2010;30(4):961-981. doi:10.1148/rg.304095755
- Bin Abd Razak HR, Bin Ali N, Howe TS. Generalized ligamentous laxity may be a predisposing factor for musculoskeletal injuries. J Sci Med Sport. 2014;17(5):474-478. doi:10.1016/j.jsams.2013.11.001
- Bin Abd Razak HR, Bin Ali N, Howe TS. Generalized ligamentous laxity may be a predisposing factor for musculoskeletal injuries. J Sci Med Sport. 2014;17(5):474-478. doi:10.1016/j.jsams.2013.11.001
- Pacey V, Nicholson LL, Adams RD, Munn J, Munns CF. Generalized Joint Hypermobility and Risk of Lower Limb Joint Injury During Sport: A Systematic Review With Meta-Analysis. Am J Sports Med. 2010;38(7):1487-1497. doi:10.1177/0363546510364838
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Diederichs G, Issever AS, Scheffler S. MR Imaging of Patellar Instability: Injury Patterns and Assessment of Risk Factors <sup/>. RadioGraphics. 2010;30(4):961-981. doi:10.1148/rg.304095755
- Golant A, Quach T, Rose J. Patellofemoral Instability: Diagnosis and Management. In: Hamlin M, ed. Current Issues in Sports and Exercise Medicine. InTech; 2013. doi:10.5772/56508
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Diederichs G, Issever AS, Scheffler S. MR Imaging of Patellar Instability: Injury Patterns and Assessment of Risk Factors <sup/>. RadioGraphics. 2010;30(4):961-981. doi:10.1148/rg.304095755
- Golant A, Quach T, Rose J. Patellofemoral Instability: Diagnosis and Management. In: Hamlin M, ed. Current Issues in Sports and Exercise Medicine. InTech; 2013. doi:10.5772/56508
- Dixit S, Deu RS. Nonoperative Treatment of Patellar Instability: Sports Med Arthrosc Rev. 2017;25(2):72-77. doi:10.1097/JSA.0000000000000149
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Diederichs G, Issever AS, Scheffler S. MR Imaging of Patellar Instability: Injury Patterns and Assessment of Risk Factors <sup/>. RadioGraphics. 2010;30(4):961-981. doi:10.1148/rg.304095755
- Bitar AC, Demange MK, D’Elia CO, Camanho GL. Traumatic Patellar Dislocation: Nonoperative Treatment Compared With MPFL Reconstruction Using Patellar Tendon. Am J Sports Med. 2012;40(1):114-122. doi:10.1177/0363546511423742
- Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y. Acute Patellar Dislocation in Children and Adolescents: A Randomized Clinical Trial: J Bone Jt Surg-Am Vol. 2008;90(3):463-470. doi:10.2106/JBJS.G.00072
- DeFroda SF, Gil JA, Boulos A, Cruz AI. Diagnosis and Management of Traumatic Patellar Instability in the Pediatric Patient. Orthopedics. 2017;40(5):e749-e757. doi:10.3928/01477447-20170602-04
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Parikh SN, Lykissas MG, Gkiatas I. Predicting Risk of Recurrent Patellar Dislocation. Curr Rev Musculoskelet Med. 2018;11(2):253-260. doi:10.1007/s12178-018-9480-5
- DeFroda SF, Gil JA, Boulos A, Cruz AI. Diagnosis and Management of Traumatic Patellar Instability in the Pediatric Patient. Orthopedics. 2017;40(5):e749-e757. doi:10.3928/01477447-20170602-04
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Diederichs G, Issever AS, Scheffler S. MR Imaging of Patellar Instability: Injury Patterns and Assessment of Risk Factors <sup/>. RadioGraphics. 2010;30(4):961-981. doi:10.1148/rg.304095755
- Golant A, Quach T, Rose J. Patellofemoral Instability: Diagnosis and Management. In: Hamlin M, ed. Current Issues in Sports and Exercise Medicine. InTech; 2013. doi:10.5772/56508
- Diduch DR, Kandil A, Burrus MT. Lateral Patellar Instability in the Skeletally Mature Patient: Evaluation and Surgical Management. J Am Acad Orthop Surg. 2018;26(12):429-439. doi:10.5435/JAAOS-D-16-00052
- Carlson VR, Boden BP, Shen A, Jackson JN, Yao L, Sheehan FT. The Tibial Tubercle-Trochlear Groove Distance Is Greater in Patients With Patellofemoral Pain: Implications for the Origin of Pain and Clinical Interventions. Am J Sports Med. 2017;45(5):1110-1116. doi:10.1177/0363546516681002
- Straume-Næsheim TM, Randsborg P-H, Mikaelsen JR, et al. Recurrent lateral patella dislocation affects knee function as much as ACL deficiency – however patients wait five times longer for treatment. BMC Musculoskelet Disord. 2019;20(1). doi:10.1186/s12891-019-2689-7
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Diederichs G, Issever AS, Scheffler S. MR Imaging of Patellar Instability: Injury Patterns and Assessment of Risk Factors <sup/>. RadioGraphics. 2010;30(4):961-981. doi:10.1148/rg.304095755
- Diduch DR, Kandil A, Burrus MT. Lateral Patellar Instability in the Skeletally Mature Patient: Evaluation and Surgical Management. J Am Acad Orthop Surg. 2018;26(12):429-439. doi:10.5435/JAAOS-D-16-00052
- Golant A, Quach T, Rose J. Patellofemoral Instability: Diagnosis and Management. In: Hamlin M, ed. Current Issues in Sports and Exercise Medicine. InTech; 2013. doi:10.5772/56508
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Diduch DR, Kandil A, Burrus MT. Lateral Patellar Instability in the Skeletally Mature Patient: Evaluation and Surgical Management. J Am Acad Orthop Surg. 2018;26(12):429-439. doi:10.5435/JAAOS-D-16-00052
- Golant A, Quach T, Rose J. Patellofemoral Instability: Diagnosis and Management. In: Hamlin M, ed. Current Issues in Sports and Exercise Medicine. InTech; 2013. doi:10.5772/56508
- Fisher B, Nyland J, Brand E, Curtin B. Medial Patellofemoral Ligament Reconstruction for Recurrent Patellar Dislocation: A Systematic Review Including Rehabilitation and Return-to-Sports Efficacy. Arthrosc J Arthrosc Relat Surg. 2010;26(10):1384-1394. doi:10.1016/j.arthro.2010.04.005
- McNeilan RJ, Everhart JS, Mescher PK, Abouljoud M, Magnussen RA, Flanigan DC. Graft Choice in Isolated Medial Patellofemoral Ligament Reconstruction: A Systematic Review With Meta-analysis of Rates of Recurrent Instability and Patient-Reported Outcomes for Autograft, Allograft, and Synthetic Options. Arthrosc J Arthrosc Relat Surg. 2018;34(4):1340-1354. doi:10.1016/j.arthro.2017.11.027
- Sanchis-Alfonso V. How to Deal With Chronic Patellar Instability: What Does the Literature Tell Us? Sports Health Multidiscip Approach. 2016;8(1):86-90. doi:10.1177/1941738115604156
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Golant A, Quach T, Rose J. Patellofemoral Instability: Diagnosis and Management. In: Hamlin M, ed. Current Issues in Sports and Exercise Medicine. InTech; 2013. doi:10.5772/56508
- Diduch DR, Kandil A, Burrus MT. Lateral Patellar Instability in the Skeletally Mature Patient: Evaluation and Surgical Management. J Am Acad Orthop Surg. 2018;26(12):429-439. doi:10.5435/JAAOS-D-16-00052
- McNeilan RJ, Everhart JS, Mescher PK, Abouljoud M, Magnussen RA, Flanigan DC. Graft Choice in Isolated Medial Patellofemoral Ligament Reconstruction: A Systematic Review With Meta-analysis of Rates of Recurrent Instability and Patient-Reported Outcomes for Autograft, Allograft, and Synthetic Options. Arthrosc J Arthrosc Relat Surg. 2018;34(4):1340-1354. doi:10.1016/j.arthro.2017.11.027
- Hinterwimmer S, Imhoff AB, Minzlaff P, et al. Anatomical two-bundle medial patellofemoral ligament reconstruction with hardware-free patellar graft fixation: technical note and preliminary results. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2013;21(9):2147-2154. doi:10.1007/s00167-013-2498-8
- Manske RC, Prohaska D. REHABILITATION FOLLOWING MEDIAL PATELLOFEMORAL LIGAMENT RECONSTRUCTION FOR PATELLAR INSTABILITY. Int J Sports Phys Ther. 2017;12(3):494-511.
- Diduch DR, Kandil A, Burrus MT. Lateral Patellar Instability in the Skeletally Mature Patient: Evaluation and Surgical Management. J Am Acad Orthop Surg. 2018;26(12):429-439. doi:10.5435/JAAOS-D-16-00052
- Manske RC, Prohaska D. REHABILITATION FOLLOWING MEDIAL PATELLOFEMORAL LIGAMENT RECONSTRUCTION FOR PATELLAR INSTABILITY. Int J Sports Phys Ther. 2017;12(3):494-511.
- Manske RC, Prohaska D. REHABILITATION FOLLOWING MEDIAL PATELLOFEMORAL LIGAMENT RECONSTRUCTION FOR PATELLAR INSTABILITY. Int J Sports Phys Ther. 2017;12(3):494-511.
- Ries Z, Bollier M. Patellofemoral Instability in Active Adolescents. J Knee Surg. 2015;28(04):265-278. doi:10.1055/s-0035-1549017
- Manske RC, Prohaska D. REHABILITATION FOLLOWING MEDIAL PATELLOFEMORAL LIGAMENT RECONSTRUCTION FOR PATELLAR INSTABILITY. Int J Sports Phys Ther. 2017;12(3):494-511.
- Saper MG, Fantozzi P, Bompadre V, Racicot M, Schmale GA. Return-to-Sport Testing After Medial Patellofemoral Ligament Reconstruction in Adolescent Athletes. Orthop J Sports Med. 2019;7(3):232596711982895. doi:10.1177/2325967119828953
- Golant A, Quach T, Rose J. Patellofemoral Instability: Diagnosis and Management. In: Hamlin M, ed. Current Issues in Sports and Exercise Medicine. InTech; 2013. doi:10.5772/56508
- Saper MG, Fantozzi P, Bompadre V, Racicot M, Schmale GA. Return-to-Sport Testing After Medial Patellofemoral Ligament Reconstruction in Adolescent Athletes. Orthop J Sports Med. 2019;7(3):232596711982895. doi:10.1177/2325967119828953
- Saper MG, Fantozzi P, Bompadre V, Racicot M, Schmale GA. Return-to-Sport Testing After Medial Patellofemoral Ligament Reconstruction in Adolescent Athletes. Orthop J Sports Med. 2019;7(3):232596711982895. doi:10.1177/2325967119828953
