- Willy, R.; et al. Patellofemoral Joint and Achilles Tendon Loads During Overground and Treadmill Running. J of Ortho & Sports PT . 2016; 46; 664-72. “...treadmill running resulted in greater Achilles tendon loading compared with overground running.“
- Gottschall JS, Kram R. Ground reaction forces during downhill and uphill running. J Biomech. 2005 Mar;38(3):445-52. “…Combined with previous biomechanics studies, our normal impact force data suggest that downhill running substantially increases the probability of overuse running injury. Our parallel force data provide insight into past energetic studies, which show that the metabolic cost increases during downhill running at steep angles.”
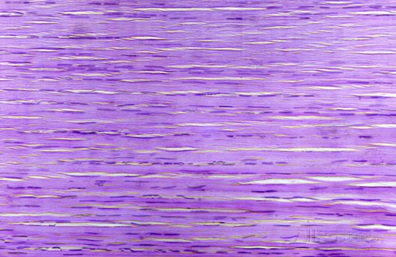
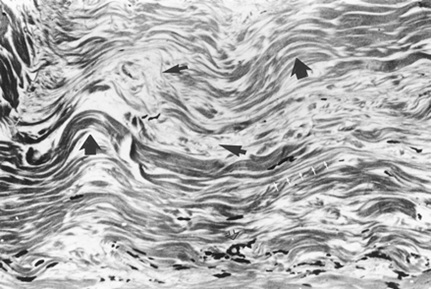
- Khan KM, Cook JL, Bonar F, Harcourt P, Astrom M. Histoathology of common tendinopathies. Update and implications for clinical management. Sports Med. 1999 Jun;27(6):393-408. Often, there is an abrupt discontinuity of both vascular and myofibroblastic proliferation immediately adjacent to the area of greatest abnormality. The most significant feature is the absnce of inflammatory cells. These observations confirm that the histopathological findings in athletes with overuse tendinopathies are consistent with those in tendinosis…”
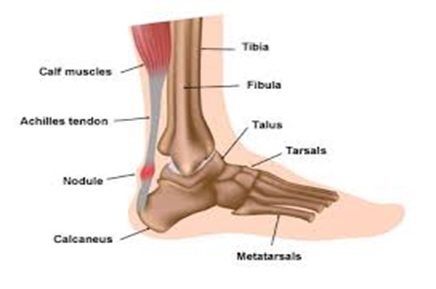
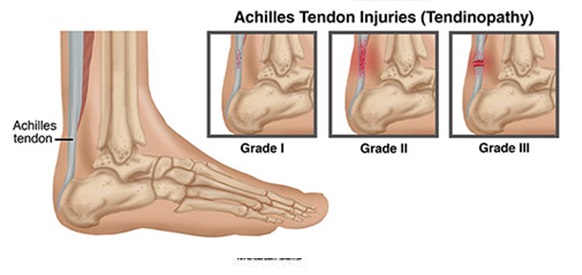
- Maffulli N. The clinical diagnosis of subcutaneous tear of the Achilles tendon. A prospective study in 174 patients. Am J Sports Med. 1998 Mar-Arp;26(2):266-70. “Both the calf squeeze and Matles tests were significantly more sensitive than the other tests…. the tests showed a high capability to detect that the Achilles tendon was intact.”
- Alfredson H, Cook J. A treatment algorithm for managing Achilles tendinopathy: new treatment options. Br J Sports Med. 2007 Apr;41(4):211-216. “…if a clinical diagnosis is not clear, ultrasonography or MRI may reveal the pathology with in the tendon….”
- Azevedo LB, et al. Biomechanical variables associated with Achilles tendinopathy in runners. Br J Sports Med. 2009 Apr;43(4):288-92) “…Altered knee kinematics and reduced muscle activit are associated with Achilles tendinopathy in runners. Rehabilitation exercises or other mechanisms (e.g. footware) that affect kinematics and muscle activity may therefore be beneficial in the treatment of runners with Achilles tendinopathy.”
- Ryan, M., Grau, S., Krauss, I., Maiwald, C., Taunton, J., & Horstmann, T. (2009). Kinematic Analysis of Runners with Achilles Mid-Portion Tendinopathy. Foot and Ankle International, 30(12), 1190–1195 “…we found an increase in eversion displacement of the sub-talar joint in runners with Achilles mid-portion tendinopathy.”
- Carcia C, Martin R, Houck J, Wukich D. Achilles pain,m stiffness, and muscle power deficits: achilles tendinitis. J Orthop Sports Phys Ther. 2010:40(9):A1-A26.
- Alfredson H, Cook J. A treatment algorithm for managing Achilles tendinopathy: new treatment options. Br J Sports Med. 2007 Apr;41(4):211-216. “…if a clinical diagnosis is not clear, ultrasonography or MRI may reveal the pathology with in the tendon….“
- Kaufman KR, et al. The effect of foot structure and range of motion on musculoskeletal overuse injuries. Am J Sports Med. 1999 Sept-Oct;27(5):585-93. “The subjects were tracked prospectively for injuries throughout training. We identified risk factors that predispose people to lower extremity overuse injuries. These risk factors include dynamic pes planus, pes cavus, restricted ankle dorsiflexion, and increased hindfoot inversion, all of which are subject to intervention and possible correction.”
- Imai K, et al. Tissue Mobilization Therapy on Achilles Tendinopathy in a Rabbit Model. Feb, 28(2)112-8. “…Biomechanical and histological findings showed that the Achilles tendons treated with ASTM had better recovery of biomechanical function that did control tendons.”
- McCormack JR, et al. Eccentric Exercise Versus Eccentric Exercise and Soft Tissue Treatment (Astym) in the Management of Insertional Achilles Tendinopathy: A Randomized Controlled Trial. Sports Health. 2016 Feb. “…Soft tissue treatment (Astym) plus eccentric exercise was more effective than eccentric exercise only at improving function during both short- and long-term follow-up periods.”
- Kaufman KR, et al. The effect of foot structure and range of motion on musculoskeletal overuse injuries. Am J Sports Med. 1999 Sept-Oct;27(5):585-93. “The subjects were tracked prospectively for injuries throughout training. We identified risk factors that predispose people to lower extremity overuse injuries. These risk factors include dynamic pes planus, pes cavus, restricted ankle dorsiflexion, and increased hindfoot inversion, all of which are subject to intervention and possible correction.”
- Voorn R. Case report: can sacroiliac joint dysfunction cause chronic Achilles tendinitis? J Orthop Sports Phys Ther. 1998 Jun;27(6):436-43.
- Mahieu NN, et al. Intrinsic risk factors for the development of achilles tendon overuse injury: a prospective study. Am J Sports Med. 2006 Feb;34(2):226-35. “…the strength of the plantar flexors and amount of dorsiflexion excursion were identified as significant predictors of an Achilles tendon overuse injury. A plantar flexor strength lower than 50.0 N.m and dorsiflexion range of motion higher than 9.0 degrees were possible thresholds for developing an Achilles tendon overuse injury.”
- Hein T, et al. Prospective analysis of intrinsic and extrinsic risk factors on the development of Achilles tendon pain in runners. Scandinavian J Med & Sci in Sports. June 2014 (3)e201-12. “…runners developing Achilles tendon pain already show differences in their lower extremity kinematics, muscular strength, and training habits. More extended knee and ankle joints lead to a more forward-shifted touchdown and higher stress on the Achilles tendon during the weight bearing”
- Franettovich Smith MM, et al. Neuromotor control of gluteal muscles in runners with achilles tendinopathy. Med Sci Sports Excerc. 2014 Mar;46(3):594-9. “…This study provides preliminary evidence of altered neuromotor control of the GMED and GMAX muscles in male runners with Achilles tendinopathy. Although further prospective studies are required to discern the causal nature of this relationship, this study highlights the importance of considering neuromotor control of the gluteal muscles in the assessment and management of patients with Achilles tendinopathy.”
- Azevedo LB, et al. Biomechanical variables associated with Achilles tendinopathy in runners. Br J Sports Med. 2009 Apr;43(4):288-92) “…Altered knee kinematics and reduced muscle activit are associated with Achilles tendinopathy in runners. Rehabilitation exercises or other mechanisms (e.g. footware) that affect kinematics and muscle activity may therefore be beneficial in the treatment of runners with Achilles tendinopathy.”
- Azevedo LB, et al. Biomechanical variables associated with Achilles tendinopathy in runners. Br J Sports Med. 2009 Apr;43(4):288-92) “…Altered knee kinematics and reduced muscle activit are associated with Achilles tendinopathy in runners. Rehabilitation exercises or other mechanisms (e.g. footware) that affect kinematics and muscle activity may therefore be beneficial in the treatment of runners with Achilles tendinopathy.”
- Habets B, Smits HW, Backx FJG, van Cingel REH, Huisstede BMA. Hip muscle strength is decreased in middle-aged recreational male athletes with midportion Achilles tendionapthy: A cross-sectional study. Phys Ther in Sport. 2017 May;25:55-61. “Compared to controls, participants with AT demonstrated 28.9% less isometric hip abduction strength (p = 0.012), 34.2% less hip external rotation strength (p = 0.010), and 28.3% less hip extension strength (p = 0.034) in the injured limb.”
- Ohberg L, Lorentzon R, Alfredson H. Eccentric training in patients with chronic Achilles teninosis: normalised tendon structure and decreased thickness at follow up. Br J Sports Med. 2004;38:8-11. “…Ultrasonographic follow up of patients with mid-portion painful chronic Achilles tendinosis treated with eccentric calf muscle training showed a localised decrease in tendon thickness and a normalised tendon structure in most patients. Remaining structural tendon abnormalities seemed to be associated with residual pain in the tendon.”
- Torstensen T, Meen H, Stiris M. The effect of medical exercise therapy on a patient with chronic supraspinatus tendinitis. Diagnostic ulatrasound-tissue regeneration: a case study. J Of Ortho & Sports Phys Ther. 1994;20(6)319-27.
- O’Neill S, Watson P, Barry S. Why are eccentric exercises effective for achilles tendinopathy? Int J Sports Phys Ther. 2015 Aug;10(4):552-62.
- Alfredson H, et al. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med. 1998 May-Jun;26(3):360-6.
- Fahlstrom M, et al. Chronic Achilles tendon pain treated with eccentric calf-muscle training. Knee Surg Sports Traumatol Arthrosc. 2003 Sep;11(5):327-33.
- Roos EM, et al. Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy–a randomized trial with 1-year follow-up. Scand J Med Sci Sports. 2004 Oct;14(5):286-95.
- Gardin A, et al. The long-term clinical and MRI results following eccentric calf muscle training in chronic Achilles tendinosis. Skeletal Radiol. 2010 May;39(5):435-42.
- Kvist M. Achilles tendon injuries in athletes. Ann Chir Gynaecol. 1991;80(2):188-201. “…Different structural faults were found in 60% of the athletes with Achilles tendon overuse injuries. Forefoot varus correlated (r = P less than 0.001) with paratenonitis.”[/note]; or
2) The gait assessment reveals grossly excessive pronation – which has been linked to the development of AT by multiple studies. 28McCrory JL, et al. Etiologic factors associated with Achilles tendinitis in runners. Med Sci Sports Exerc. 1999 Oct;31(10):1374-81.“…arch index were found to be significant discriminators…between runners afflicted with Achilles tendinitis and runners who had no history of overuse injury.“
- Reule CA, et al. Spatial orientation of the subtalar joint axis is different in subjects with and without Achilles tendon disorders. Br J Sports Med. 2011 Oct;45(13):1029-34. “…the mean deviation angle (of the ankle joint) in people with Achilles tendon pathologies is significantly more oblique than in people without. This finding indicates that the spatial orientation of the (ankle joint) is related to the incidence of overuse injuries of the Achilles tendon in the investigated sample” (long-distance runners)
- Mayer F, et al. Effects of short-term treatment strategies over 4 weeks in Achilles tendinopathy. Br J Sports Med. 2007 Jul;41(7):e6. “...Most patients with AT experience a reduction in pain after only 4 weeks of differentiated, non-surgical treatment consisting of physiotherapy or semi-rigid insoles.”
- Donoghue OA, et al. Orthotic control of rear foot and lower limb motion during running in participants with chronic Achilles tendon injury. Sports Biomech. 2008 May;7(2):194-205. “…participants reported between 50 and 100% (average 92%) relief from symptoms with the use of orthoses.”[/note] and altering neuromuscular recruitment patterns of the calf muscles (which may be dysfunctional in runners with chronic AT). 32Wyndow N, et al. Neuromotor control of the lower limb in Achilles tendinopathy: implications for foot orthotic therapy. Sports Med. 2010 Sep 1;40(9):715-27. “…it is possible that foot orthoses may aid to normalize intratendinous loads via altering neuromotor activity in the triceps surae (calf muscle) in AT.”
- Sinclair J, Isherwood J, Taylor PJ. Effects of foot orthoses on Achilles tendon load in recreational runners. Clinical Biomech, 2014 Sept;29(8):956-8. “…The results indicate that running with foot orthotics was associated with significant reductions in Achilles tendon load compared to without orthotics… the current investigation suggests that via reductions in Achilles tendon load, foot orthoses may serve to reduce the incidence of chronic Achilles tendon pathologies in runners.”
- Tumilty S, et al. Low level laser treatment of tendinopathy: a systematic review with meta-analysis. Photomed Laser Surg. 2010 Feb;28(1):3-16. “…LLLT can potentially be effective in treating tendinopathy when recommended dosages are used. The 12 positive studies provide strong evidence that positive outcomes are associated with the use of current dosage recommendations for the treatment of tendinopathy.”
- Bjordal JM, Lopes-Martins RA, Iversen VV. A radomised, placebo controlled trial of low level laser therapy for activated Achilles tendinitis with microdialysis measurement of peritendinous prostaglandin E2 concentrations. Br J Sports Med. 2006 Jan;40(1):76-80. “LLLT at a dose of 5.4 J per point can reduce inflammation and pain in activated Achilles tendinitis.”
- Stergioulas A, et al. Effects of low-level laser therapy and eccentric exercises in the treatment of recreational athletes with chronic achilles tendinopathy. Am J Sports Med. 2008 May;36(5):881-7. “…Low-level laser therapy, with the parameters used in this study, accelerates clinical recovery from chronic Achilles tendinopathy when added to an EE regimen. For the LLLT group, the results at 4 weeks were similar to the placebo LLLT group results after 12 weeks.”
- Tumilty S, et al. Clinical effectiveness of low-level laser therapy as an adjunct to eccentric exercise for the treatment of Achilles’ tendinopathy: a randomized controlled trial. Arch Phys Med Rehabil. 2012 May;93(5):733-9. “…The clinical effectiveness of adding LLLT to eccentric exercises for the treatment of Achilles’ tendinopathy has not been demonstrated using the parameters in this study.”
- Bjordal J, et al. The anti-inflammatory mechanism of low level laser therapy and its relevance for clinical use in physiotherapy. J Phys Ther Rev 2013 Jul;15(4):286-93. “…Red and near infrared LLLT administered with mean laser output of 2.5–100 mW, irradiation times of 16–600 s and doses of 0.6–9.6 J reduces inflammation significantly, and is equally effective as NSAIDs in animal laboratory studies. “
- MacLellan GE, Vyvyan B. Management of pain beneath the heel and Achilles tendonitis with visco-elastic heel inserts. Br J Sports Med. 1981 Jun;15(2):117-21.
- Lowdon A, Bader DL, Mowat AG. The effect of heel pads on the treatment of Achilles tendinitis: a double blind trial. Am J Sports Med. 1984 Nov-Dec;12(6):431-5. “…the claimed benefit of viscoelastic pads widely used by athletes was not substantiated”
- Roos EM, et al. Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy–a randomized trial with 1-year follow-up. Scand J Med Sci Sports. 2004 Oct;14(5):286-95. “…the claimed benefit of viscoelastic pads widely used by athletes was not substantiated”
- de Vos RJ, et al. The additional value of a night splint to eccentric exercises in chronic midportion Achilles tendinopathy: a randomised controlled trial. Br J Sports Med. 2007 Jul;41(7):e5. “…A night splint is not beneficial in addition to eccentric exercises in the treatment of chronic midportion Achilles tendinopathy.“
- Petersen W, Welp R, Rosenbaum D. Chronic Achilles teninopathy: a prospective randomized study comparing the therapeutic effect of eccentric training, the AirHeel brace, and a combination of both. Am J Sports Med. 2007 Oct;35(10):1659-67. “…The AirHeel brace is as effective as eccentric training in the treatment of chronic Achilles tendinopathy. There is no synergistic effect when both treatment strategies are combined.”
- Brown D, Lauber CA. Evidence based guidelines for utilisation of dexamethasone iontophoresis. Internat J Athl Ther Training. 2011;16(4):33‐36.
- Neeter C, et al. Iontophoresis with or without dexamethazone in the treatment of acute Achilles tendon pain. Scand J Med & Sci in Sports. 2003 Dec;13(6):376-82. “…positive effects from using iontophoresis with dexamethazone were found in the treatment of patients with acute Achilles tendon pain.”
- Inoue M, et al. The effect of electroacupuncture on tendon repair in a rat Achilles tendon rupture model. Acupunct Med. 2015 Feb;33(1):58-64. “…The marked increase in cell count and growth factor expression as well as increased tendon strength in the EA group suggest that EA may be a useful method for promoting tendon repair.”
- Andres M, Murrell G. Treatment of Tendinopathy: What works, what does not, and what is on the horizon. Clin Orthop Relat Res. 2008 Jul;466(7):1539-54.” This treatment modality has been extensively studied over the past 10 years, and there is a great deal of variability in the data…Further evidence is needed to justify the use of ESWT in Achilles tendinopathy and patellar tendinopathy.”
- Rompe JD, Nafe B, Furia JP, Maffulli N. Eccentric loading, shock-wave treatment, or a wait-and-see policy for tendinopathy of the main body of tendo Achillis: a radomized controlled trial. Am J Sports Med. 2007 Mar;35(3):374-83.
- Magnussen RA, Dunn WR, Thomson AB. Nonoperative treatment of midportion Achilles tendinopathy: a systematic review. Clin J Sport Med. 2009 Jan 19(1):54-64.
- Astrom M, Westlin N. No effect of piroxicam on achilles tendinopathy. A randomized study of 70 patients. Acta Orthop Scand. 1992 Dec;63(6):631-4. “…No differences were seen between the groups at any time during the study.”
- McLauchlan GJ, Handoll HH. Interventions for treating acute and chronic Achilles tendinitis. Cochrane Database Syst Rev. 2001;(2):CD000232. “…There was weak but not robust evidence from three trials of a modest benefit of NSAIDs for the alleviation of acute symptoms… The results of a comparison of glycosaminoglycan sulfate with a NSAID were inconclusive.”
- Almekinders LC, Temple JD. Etiology, diagnosis, and treatement of tendonitis: an analysis of the literature. Med Sci Sports Exerc. 1998 Aug;30(8):1183-90. “…Twenty-three studies on steroid injections were found. Eight were prospective and placebo controlled studies, with three showing beneficial effects of the injection at follow-up. It was concluded that much of the pathology and etiology of tendonitis remains unclear.”
- Smidt N, et al. Corticosteroid injections, physiotherapy, or a wait-and see policy for lateral epicondylitis: a randomised controlled trial. Lancet. 2001 Feb 23;359(9307):657-62.
- Fredberg U. Local corticosteroid injection in sport: review of literature and guidelines for treatment. Scand J Med Sci Sports. 1997 Jun;7(3):131-9. “Injection of corticosteroid inside the tendon has a deleterious effect on the tendon tissue and should be unanimously condemned.”
- Gill SS, et al. Fluoroscopicallly guided low-volume peritendinous corticosteroid injection for Achilles tendinopathy. A safety study. J Bone Joint Surg Am. 2004 Apr;86-A(4):802-6. “This… study establishes the safety of low-volume injections of corticosteroids for the treatment of Achilles tendinopathy when the needle is carefully inserted into the peritendinous space under direct fluoroscopic visualization.”
- Shrier I, Matheson GO, Hohl HW 3rd. Achilles tendonitis: are corticosteroid injections useful or harmful? Clin J Sport Med. 1996 Oct;6(4):245-50. “There are insufficient published data to determine the comparative risks and benefits of corticosteroid injections in Achilles tendonitis. The decreased tendon strength with intratendinous injections in animal studies suggests that rupture may be a potential complication for several weeks following injection.”
- Gambito Ed, et al. Evidence on the effectivenss of topical nitroglycerin in the treatment of tendinopathies: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2010 Aug;91(8):1291-305. “In chronic tendinopathies, there is strong evidence for NTG in relieving pain during activities of daily living, and increasing tendon strength. Further studies are needed to explore the role of this promising intervention in all phases of tendinopathies.”
- Paoloni JA, et al. Topical glyceryl trinitrate treatment of chronic noninsertional achilles tendnopathy. A randomized double-blind, placebo-controlled trial. J Bone Joint Surg Am. 2004 May;86-A(5):916-22. “Topical glyceryl trinitrate significantly reduced pain with activity and at night, improved functional measures, and improved outcomes in patients with Achilles tendinopathy.”
- Kane TP, Ismail M, Calder JD. Topical glyceryl trinitrate and noninsertional Achilles tendinopathy: a clinical and cellular investigation. Am J Sports Med. 2008 Jun;36(6):1160-3. “Topical glyceryl trinitrate significantly reduced pain with activity and at night, improved functional measures, and improved outcomes in patients with Achilles tendinopathy.”
- Paoloni JA, Murrell GA. Three-year followup of topical glyceryl trinitrate treatment of chronic noninsertional Achilles tendinopathy. Foot Ankle Int. 2007 Oct;28(10):1064-8.
- Paoloni JA, Murrell GA. Three-year followup of topical glyceryl trinitrate treatment of chronic noninsertional Achilles tendinopathy. Foot Ankle Int. 2007 Oct;28(10):1064-8. “Topical glyceryl trinitrate treatment has demonstrated efficacy in treating chronic noninsertional Achilles tendinopathy, and the treatment benefits continue at 3 years. Significant differences in asymptomatic patient outcomes for the glyceryl trinitrate group continue at 3 years, and this is confirmed by the effect size estimate. This suggests that the mechanism of action of topical glyceryl trinitrate on chronic tendinopathies is more than an analgesic effect.”
- Ohberg L, Alfredson H. Ultrasound guided sclerosis of neovessels in painful chronic Achilles tendinosis: pilot study of a new treatment. Br J Sports Med. 2002 Jun;36(3):173-5. “Sclerosing neovessels appears to be an effective treatment for painful chronic Achilles tendinosis, suggesting that neovessels play a key part in causing chronic tendon pain.”
- Alfredson H, Ohberg L. Sclerosing injections to areas of neo-vascularisation reduce pain in chronic Achilles tendinopathy: a double-blind randomised controlled trial. Knee Surg Sports Traumatol Arthrosc. 2005 May;13(4):338-44. “After completion of the study, treatment with Polidocanol injections (Cross-over in group B and additional treatments in group A) resulted in 10/10 and 9/10 satisfied patients in group A and B, respectively. In summary, injections with the sclerosing substance Polidocanol have the potential to reduce tendon pain during activity in patients with chronic painful mid-portion Achilles tendinopathy.”
- Lind B, Ohberg L, Alfredson H. Sclerosing polidocanol injections in mid-portion Achilles tendinosis: remaining good clinical results and decreased tendon thickness at 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2006 Dec;14(12):1327-32. “treatment with sclerosing polidocanol injections in patients with chronic painful mid-portion Achilles tendinosis showed remaining good clinical results at a 2-year follow-up.”
- van Sterkenburg MN, et al. Less promising results with sclerosing ethoxysclerol injections for midportion achilles tendinopathy: a retrospective study. Am J Sports Med. 2010 Nov;38(11):2226-32. “Our study did not confirm the high beneficial value of sclerosing neovascularization in patients with midportion Achilles tendinopathy. Despite the retrospective design of our study, we consider it important to stress that injection of Ethoxysclerol may not be as promising as was thought.”
- van Sterkenburg MN, et al. Less promising results with sclerosing ethoxysclerol injections for midportion achilles tendinopathy: a retrospective study. Am J Sports Med. 2010 Nov;38(11):2226-32. “Our study did not confirm the high beneficial value of sclerosing neovascularization in patients with midportion Achilles tendinopathy. Despite the retrospective design of our study, we consider it important to stress that injection of Ethoxysclerol may not be as promising as was thought.”
- Ryan M, Wong A, Taunton J. Favorable Outcomes After Sonographically Guided Intratendinous Injection of Hyperosmolar Dextrose for Chronic Insertional and Midportion Achilles Tendinosis. AJR 2010;194:1047-53. “Dextrose injections appear to present a low-cost and safe treatment alternative with good long-term evidence for reducing pain from pathology at either the insertion or midportion of the Achilles tendon.“
- Yelland JM, et al. Prolotherapy injections and eccentric loading exercises for painful Achilles tendinosis: a randomised trial. Br J Sports Med. 2011 Apr;45(5):421-8. “For Achilles tendinosis, prolotherapy and particularly ELE combined with prolotherapy give more rapid improvements in symptoms than ELE alone but long-term VISA-A scores are similar.”
- Meakins, A. (2015, October 29). Prolotherapy… Is it as ‘sweet’ as it sounds??? Retrieved December 5, 2015, from https://thesportsphysio.wordpress.com/2012/11/20/prolotherapy-is-it-as-sweet-as-it-sounds/
- Rabago D, Slattengren A, Zgierska A. Prolotherapy in Primary Care Practice. Prim Care. 2010 Mar;37(1):65-80.
- Andres M, Murrell G. Treatment of Tendinopathy: What works, what does not, and what is on the horizon. Clin Orthop Relat Res. 2008 Jul;466(7):1539-54.”Current data support the use of eccentric strengthening protocols, sclerotherapy, and nitric oxide patches, but larger, multicenter trials are needed to confirm the early results with these treatments. Preliminary work with growth factors and stem cells is promising, but further study is required in these fields. Surgery remains the last option due to the morbidity and inconsistent outcomes. The ideal treatment for tendinopathy remains unclear.”
- de Vos RJ, et al. Platelet-rich plasma injection for chronic Achilles tendinopathy: a randomized controlled trial. JAMA. 2010 Jan 13;303(2):144-9. “Among patients with chronic Achilles tendinopathy who were treated with eccentric exercises, a PRP injection compared with a saline injection did not result in greater improvement in pain and activity.”
- Tsikopoulos K, et al. The clinical impact of platelet-rich plasma on tendinopathy compared to placebo or dry needling injections: A meta-analysis. Phys Ther in Sport. Jan 2016.17:87-94.
- Yee Lui PP. Stem cell technology for tendon regeneration: current status, challenges, and future research directions. Stem Cells Cloning. 2015;8:163-174. “the advantages and limitations of using different types of stem cells compared to terminally differentiated cells for tendon tissue engineering. The safety and efficacy of application of stem cells and their modified counterparts for tendon tissue engineering were then summarized after a systematic literature search in PubMed. The challenges and future research directions to enhance, optimize, and standardize stem cell-based therapies for augmenting tendon repair were then discussed.”
- Testa V, et al. Management of Achilles tendinopathy by ultrasound-guided percutaneous tenotomy. Med Sci in Sports Exerc. 2002, 34(40):573-580. “Percutaneous longitudinal ultrasound-guided internal tenotomy is simple, can be performed on an outpatient basis, requires minimal follow-up care, does not hinder further surgery should it be unsuccessful, and, in our experience, has produced no significant complications. It should be considered in the management of chronic Achilles tendinopathy after failure of conservative management. However, patients should be advised that, if they suffer from diffuse or multinodular tendinopathy or from pantendinopathy, a formal surgical exploration with stripping of the paratenon and multiple longitudinal tenotomies may be preferable.”
- Alfredson H, Cook J. A treatment algorithm for managing Achilles tendinopathy: new treatment options. Br J Sports Med. 2007 Apr;41(4):211-216. “Percutaneous tenotomy resulted in 75% of patients reporting good or excellent results after 18 months.“
- Andres M, Murrell G. Treatment of Tendinopathy: What works, what does not, and what is on the horizon. Clin Orthop Relat Res. 2008 Jul;466(7):1539-54. “Many studies evaluate various forms of surgery to treat Achilles tendinopathy…The results vary between studies and appear to correlate with the extent of tendon damage.”
- Morberg P. Long-term results after surgical management of partial Achilles tendon ruptures. Scand J Med Sci Sports. 1997 Oct;7(5):299-303. The conclusion of this study is that partial Achilles tendon ruptures are often difficult to treat and only two out of three patients can be expected to obtain satisfactory results after surgical treatment.”
- Paavola M, et al. Surgical treatment for chronic Achilles tendinopathy: a prospective seen month follow up study. Br J Sports Med. 2202 June;36(3):178-82. “Surgical treatment of chronic Achilles tendinopathy gives good and acceptable short term results. A lower complication rate and a trend to better recovery was observed in patients with peritendinous adhesions only than in those with peritendinous adhesions combined with an intratendinous lesion.”
- Khan W, et al. Analysing the outcome of surgery for chronic Achilles tendinopathy over the last 50 years. World J Orthop. 2015 Jul 18;6(6):491-497. “We conclude that although the success rate of surgery for chronic Acilles tendinopathy described in the literature has fallen over the last 50 years, this is probably due to a more rigorous methodology of the studies.”
- Tallon C, et al. Outcome of surgery for chronic Achilles tendinopathy. A critical review. Am J Sports Med. 2001 May-Jun;29(3):315-20. “Achilles tendinopathy is often treated surgically after failure of nonoperative management, but results are not uniformly excellent…..Study methods may influence reported surgical outcome, and we suggest guidelines for improving study design in this area of clinical research. We acknowledge that study methods have improved over the course of the past 20 years.”
Additional Information
Contact Us Today
Phone: 802.399.2244
Fax: 802.497.2366
Get Started
VASTA Performance Training and Physical Therapy
358 Dorset Street
South Burlington, VT 05403
1185 Shelburne Rd
South Burlington, VT 05403
802-399-2244
80 S Main Street, Suite #7
Waterbury, VT 05676
802-882-8538
32 Cottonwood Drive
Suite 100
Williston, VT 05495
802-764-0046
5301 South Dixie Hwy
West Palm Beach, FL 33405
802-655-5100
South Burlington, VT 05403
1185 Shelburne Rd
South Burlington, VT 05403
802-399-2244
80 S Main Street, Suite #7
Waterbury, VT 05676
802-882-8538
32 Cottonwood Drive
Suite 100
Williston, VT 05495
802-764-0046
5301 South Dixie Hwy
West Palm Beach, FL 33405
802-655-5100




Leave a Reply
Want to join the discussion?Feel free to contribute!