Introduction
Over the past 40-50 years, the sport of running has gone through quite a bit of change. The popularity of competitive running in America enjoyed a ‘boom’ in the early 1970’s. Frank Shorter won the Olympic Gold in the 1972 Marathon. Ron Hill (an English runner) won the Boston Marathon in 1970. Other competitive runners such as Bill Rodgers, Steve Prefontaine (and his coach Bill Bowerman) raised the ‘visability’ and popularity of running. This trend of rising popularity has waxed and waned a bit over the years, but overall remains. The number of ‘regular runners’ (defined as running > 50 x / year) increased 8.2% from 2010 to 2011 1 The pictures below are of the Starting line for the NY city Marathon from 1970 (left) and 2016 (right).


The ‘typical’ runner has changed dramatically over this same period of time. Runners in 70’s were dedicated runners. They were aiming to win. They were ‘primary runners’ – i.e. they weren’t cross-fitters who wanted to run on the side. They weren’t running to get into shape for lacrosse season. They were pure runners. There weren’t any ‘couch to marathon in 16 weeks’ participants, and there weren’t any ‘biggest loser’ participants. They were skinny (for the most part), male (> 75%) and singularly focused on running.
Modern day runners are a different animal. We now have > 60 Million runners in this country. Most are ‘recreational’ – they run to participate, not to win. Most participate in some sort of cross-training. The majority (54%) are female; And, they come in all shapes, sizes, ages, and abilities.
I bring this up for one reason. We will discuss the fact that, in spite advances in training approaches, shoe technology and rehabilitation, injury rates, among runners has stayed fairly ‘stable’ over the last 40-50 years. We believe we know (now) much more about what leads to injury, but statistics will tell us that runners continue to get injured every bit as often. I believe this is for 3 reasons:
1) Runners are different (as explained above)
2) The ‘science’ of preventing running injuries faces an up hill battle with the ‘hype’ that is pervasive is popular media, running magazines, blogs, company advertisements and the like.
3) As with most things – common execution lags behind the accumulation of good science. We now have a good bit of knowledge and insight into what underlies many repetitive stress injuries associated with running. The past ~ 10 years or so has been very productive at weeding through misconception, prejudice and assumptions to provide us with good objective data to base our recommendations on. Popular adaption of these recommendations will (always) lag behind the science.
Before we explore that science to explain why runners get hurt, let’s look at what injuries runners are getting, and how often.
Injury Rates
Depending on where you look, injury rates for runners can be highly variable. This is due to variability in defining an ‘injury’. Is an injury anything that hurts and effects your performance? Is it anything that the runner seeks medical attention for?
Or is it something that prohibits running altogether?
If you define it as something that causes some level of discomfort and effects your training in any way (e.g. you can’t run as much, or as hard, or at all, etc) than most experts agree that the number is somewhere around 70-80%.
That means that 70-80% of all runners will experience an injury in a given year. That’s a lot!
Many ‘detractors’ will point to that and say ‘hey man you shouldn’t run, it’s bad for your knees’… or ‘runners are always getting hurt’… ‘it’s bad for you’. Let’s be clear however, running is GOOD for you. Any and all forms of regular, moderately intense exercise is extraordinarily good for you!
Performing at least 150 minutes of moderate intensity exercise (such as running!) per week is associated with a number of health benefits, including a 40% reduced risk of heart disease, a 50% reduced risk of type II diabetes, a 60% reduced risk of some more aggressive types of cancer, just to name only a few. There is even evidence that regular exercise improves depression as effectively as Prozac or Behavioral Therapy. 2
“If exercise could be packed in a pill, it would be the single most widely prescribed and beneficial medicine in the nation.” —Robert H. Butler, M.D. Director, National Institute on Aging
Many have argued, convincingly, that we have evolved to be runners. We are built to run (even, we were ‘Born to Run’3). Homo erectus, emerging nearly 2 million years ago, is credited with being the first endurance runner. 4
Let’s make one thing clear (occasional sore knees aside) running is a good thing. We need to spend more time figuring out how to get more people running, and keep more people running, and less time arguing that ‘running is bad for you’.
In order to do so, we must (unfortunately) weed through a sea of nonsense. Let’s begin…
Top Running Related Injuries
The most common injuries that effect runners include:
- Medial Tibial Stress Syndrome – Medial Tibial Stress Syndrome (MTSS) refers to pain along the inside of the shin bone and is often referred to as ‘Shin Splints’. A group of muscles that help control our foot and ankle mechanics originate from this bone. The repetitive strain associated with loading these muscles causes stress to the attachment site along the bone. This may lead to inflammation at this attachment site, a stress reaction, or a full-blown stress fracture. See here for more details about MTSS.
- Achilles Tendonopathy – Achilles Tendonopathy (AT) is more common in men than woman. It is most common in middle-aged runners, but can occur at any age. On average, 50% of runners will experience Achilles tendon pain at some point in their careers, and many runners will ‘battle’ AT recurrances throughout their careers. However, our understanding of AT has improved greatly over the past decade. New treatment approaches hold promise for breaking that cycle. See here for more details about AT.
- Iliotibial Band Syndrome – Iliotibial Band (ITB) Syndrome refers to an irritation of the band of connective tissue that runs along the outside of the thigh. Most commonly, this includes an inflammation around the bottom of the band, about an inch or two above the knee joint. This is so common, it is often referred to as ‘Runners Knee’. See here for more details about ITB Syndrome.
- Plantar Fasciitis – Plantar Fasciitis (PF) is a diagnosis that runners dread. This is mostly because of its reputation to linger – PF can ‘haunt’ you for a year or more, especially if you are resistant to changes in your training routine. It is more common in runners older than 40, but can occur at any age, especially in response to rapid changes in training volume and/or intensity. See here for more details about PF.
- Patellofemoral Pain Syndrome – Patellofemoral Pain (PFP) and/or Patellar Tendonitis cause pain in, and around, the front of the knee. This is very common in runners, especially young runners. Frustratingly, it is estimated that 70-90% of all cases have recurrent or chronic pain; and, recent research suggests that having PFPS as a younger individual may predispose you to patellofemoral osteoarthritis later in life. However, there is a slew of new research suggesting promising new
 avenues to the management of PFP in runners. See here for more details.
avenues to the management of PFP in runners. See here for more details.
In addition to these ‘Top 5’, there are a whole host of other familiar foes – Hamstring Strains, Calf Strains, Muscle Cramps, Lateral Hip
Pain / ‘Trochanteric Syndrome’, Low Back Pain, etc. The point is – running is good for you! But, it can be rough on your body.
When we discuss why running leads to injury, we look at 2 broad categories – Biomechanical Issues & Training Errors.
Shoe is a ‘sort of’ 3rd category (is the ‘wrong’ shoe a biomechanical problem? Or a training error?)… See below for an in depth conversation about running shoes or click here for a discussion about whether to even wear shoes at all!
While we spend more time looking at how to improve the mechanics of running, it is important to note that most experts agree that ~ 70% of running related injuries are directly associated with some sort of training error. We will briefly touch on a few common mistakes.
Training Errors
This is a hugely in-depth topic and all highly competitive runners should consider working with a running coach. Additionally, it is important to remember that an ‘error’ for one person may not be for another based on factors such as running history, injury history, goals, etc. With that said, there are a few considerations that nearly all runners should weigh when developing a training regimen. Consider, an overriding theme: Our bodies will adapt to slow incremental changes is stress. Our bodies will react to sudden changes in stress. We must remember to give our bodies time to adapt to the stresses we plan to place on them. The human body is capable of amazing things, but the ‘adaptation’ required to perform at extremes takes time. With training, we are looking to maximize adaptation and avoid reaction.
Some recommendations:
- Employ a conscious recovery strategy – Periodization of training, appropriate rest days (especially the day after longer runs), proper fueling, soft tissue recovery (foam rolling, massage, etc), proper sleep, stress management, etc… All of these considerations play a role in recovery. ‘Recovery’ is not just taking an off-day every week; it’s much more than that.
- Strength Train 2x/week – Yes, every runner should incorporate some strength training into their routine, both to improve performance, AND to reduce injury risk. Click here for details, and here for some examples of ‘good exercises’ for runners. (This is by no means comprehensive. It is simply a taste of the ‘type’ of exercises runners should incorporate to give the reader some insight into the foundational theory that drives exercise choice) Exercise choice, dosage and pace of progression is highly individualized based on a patients exercise foundation, running history, injury history, performance goals, etc. For those with specific performance goals in mind, or with a complex injury history, you would do well to meet with a Sports Physical Therapist for a detailed running assessment and an individualized program (click here to request an appointment with a VASTA Physical Therapist).
- Avoid excessive reliance on speed, hill or stride work. Especially for the distance runner, this type of intensity / drill training should generally account for < 30% of your total weekly volume.
- When considering ‘loads’ (in an attempt to avoid sudden increases in training load) we must consider the ‘external’ loads (e.g. how many miles?, how fast? How much weight was lifted, etc…) and the ‘internal loads’ – how hard did it feel? (e.g. ‘Rate of Perceived Exertion’ (RPE)? Heart Rate?) A consideration for both of these factors is important. This is the foundation for what Tim Gabbett refers to as ‘exertional minutes’. Internal Loads (RPE) x External Loads (Total Volume) = Total Exertional Minutes. This makes sense right? 5 ‘hard’, ‘fast’ miles may impart a higher training load than 8 ‘easy’ miles. The trouble is, many runners only track their total volume (‘external loads’) and thus set them selves up for a sudden bump in overall training load when they introduce drills that incorporate intensity changes without properly adjusting their volume.
- Consider the 10% Rule. To avoid sudden increases in total weekly ‘loads’, general recommendations are typically to avoid an increase in training load (from one week to another) that exceed 10% of total ‘Exertional Minutes’. When weekly volume changes exceed 10%, injury risk appears to rise considerably. While this is an ‘ok’ rule of thumb for runners mid-season, it is likely too conservative for athletes just starting up a training routine or returning from an injury.
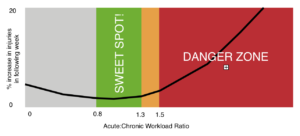
- Consider your Acute:Chronic ratio. Perhaps a ‘better’ way to avoid sudden increases in training loads is to consider this ration. Your ‘chronic’ training load is basically a ‘rolling average’ of the past 4-6 weeks of training. This attempts to more accurately reflect the runners current state of ‘fitness’ in the face weekly fluctuations that may be present in a well structured training progression. Generally, a ration of .8 > 1.3 is considered the ‘sweet spot’. Exceeding 1.5 (representing a load 1.5 times what you are ‘prepared for’) appears to elevate injury risk. Exceeding 2.0 (representing a load 2 times what you are ‘prepared for’) appears to greatly elevate injury risk.
There many other factors to consider as well – How to properly periodize your training program… When to veer off the training path if you’re feeling ‘off’ (e.g. fatigued, heavy, ‘just not right’)… How to convince yourself to take some proactive rest when little pains surface (the kind that foreshadows a big blow-up). Taking 2-3 days of rest in response to early signs of an injury, in order to prevent the kind of big inflammatory response that could necessitate 4 weeks of rest, makes all the sense in the world – on paper. But, it is hard to do. This is why a (good) coach can be essential. To help make good decisions.
Now, let’s leave the topic of training errors and dissect the mechanics of running a bit.
Mechanics of Running
The mechanics of running, at it’s core, is very simple. It is repetitively hopping from one foot to the other. That is what differentiates running from speed walking – a ‘flight phase’. 2 feet are never on the ground at the same time. There is a period (sometimes brief) between ‘push off’ (on one foot) and ‘initial contact’ on another.
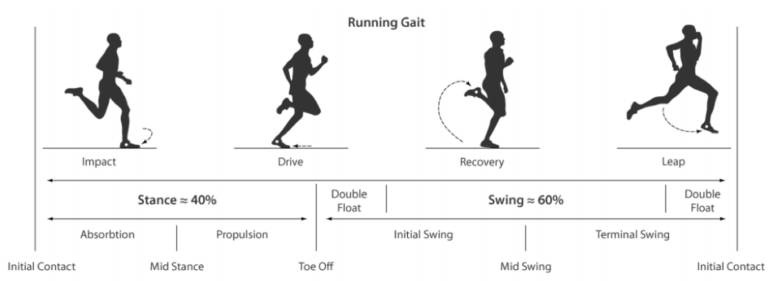
Let’s discuss a few operational definitions. Our first contact with the ground it referred to as ‘initial contact’ – thus beginning the ‘stance phase’ of gait. Immediately after, we experience the ‘loading response’. This is not when the foot just barely makes contact. Rather, it is the stage when the lower limb is beginning to accept load (typically a few milliseconds after initial contact). Next the leg moves into ‘mid-stance’ phase (with the leg directly under the body), then into it’s ‘propulsive phase’, then ‘heel rise’, and then ‘terminal stance’ phase and off the ground. The ‘swing phase’ begins with a brief periods of ‘triple extension’ (the hip, knee and ankle all in extension). The leg then begins it’s recovery and swings forward to ‘mid-swing’ and then ‘terminal swing’ just before ‘initial contact’.
While the entire stride cycle is important, injuries are more easily associated with break down during the ‘stance phase’ (especially the early portions). Thus we will look closely at impact and the ‘loading response’. The following graph is a typical representation of impact loads during running.

The line begins at ‘initial contact’ and the mini ‘blip’ on the far left represents the ‘loading response’. It is sometimes referred to at the impact transient. The two hill tops represent peak ‘Vertical Impact’ or ‘Ground Reactive Force’ (GRF). The peak on the Left represents the peak ‘passive’ impact (load being transmitted up the leg from impact with the ground) and the peak on the right represents the ‘active’ impact from the leg driving it’s self across the ground during the ‘propulsive phase’.
An important factor to note is the slope of the line of the far left. This indicates the rate of impact during the ‘loading response’.
These terms carry significant importance when discussing running related injuries. There is one other concept that is important to discuss before getting to specifics on reducing running injuries.
During the initial contact and most of the ‘loading response’ (especially in runners who heel strike) we experience what is called the breaking impulse. There is a brief moment that negatively impacts our speed.
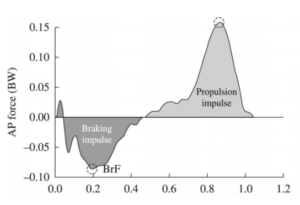
This is immediately followed by a ‘propulsive impulse’. If the ‘breaking impulse’ and the ‘propulsive impulse’ are equal, speed stays constant. To run faster, you must either 1) reduce the breaking impulse, 2) increase the propulsive impulse, or 3) both.
Also, consider, to run more efficiently at a set pace, the breaking impulse can be reduced, thus reducing the propulsion impulse (active work) required to maintain pace. Got it?
OK, now let’s look at biomechanics.

Planes of Movement
When we look at how running mechanics ‘break down’, we like to ‘categorize’ the issues into one of 3 biomechanical ‘planes’:

In general running is a Sagittal Plane movement. So when optimizing efficiency in runners we can consider 2 very general categories of considerations:
1) How to move efficiently in The Sagittal Plane – We strive to achieve the right ‘proportions’ of contribution from all joints (trunk, hip, knee, ankle). Common problems may include overstriding, insufficient hip extension during push off, ineffective trunk lean (too much or too little).
AND
2) How to minimize sloppy movement in the Frontal and Transverse plane – Runners should train to minimize movement in these planes as it (usually) represents wasted energy, and may make the athlete more prone to certain injuries.
Biomechanical Errors
In an attempt to shed some light on how we break down these various plane of movement with our runners, let’s look at a few very common issues in each plane.

Sagittal Plane
Some common Sagittal Plane problems include:
- Over striding
- Improper ankle position at initial contact
- Excessive vertical displacement (i.e. “Bounce”)
Over striding essentially means that ‘loading response’ takes place with the ground contact in front of the bodies center of mass.
With over striding we see increased GRF, increased loading rates, excessive ankle dorsiflexion, and impaired knee flexion at impact. All of these factors are associated with an increased risk of injury.
Just as one example, consider the graph to the right.
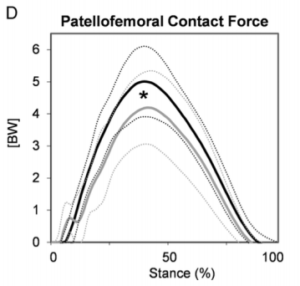
This looks at compressive forces under the knee cap while running. The light grey line represents a forefoot strike pattern. Dark Grey represents a heel striker. The very top dotted line represents a heel striker who is over striding – the difference is BIG.
Overstriding is associated with an increased chance of anterior knee pain, 5 future knee injury 6, stress fracture 7 8 It sets the runner up for future knee injury 9
Not only that, but it’s inefficient! Over striding increases the breaking impulse. Remember, this means more work required from the runner just to maintain current speed.
Improper ankle position at initial contact can lead to a number of issues. Too much ankle dorsiflexion (toe elevated) can cause anterior compartment syndrome 10 tibial stress fractures and plantar fasciitis 11 12
Too much plantar flexion (toes pointed down) by contrast can lead to Achilles tendon injury 13 14 15 16 and foot (metatarsal) fractures 17 18 19

Excessive “bounce” can also be a problem. As you can imagine, this leads to increased GRF and load rates, increasing risk for ‘impact injuries’ such as stress fracture. 20 21 22
Also, it is inefficient! Running is all about forward movement. All energy spent propelling your body up into the air is wasted energy. Watch almost any world-class runner and you will see very little up & down movement.
There are a slew of other considerations to look at in the sagittal plane – proper knee flexion at initial contact, knee flexion at mid-stance,
hip extension at terminal stance, hip & knee flexion during swing phase, trunk lean, etc… For those looking for an in-depth assessment of there gait, please click here for more information about our runner’s assessment, or contact us to set up an appointment.

Frontal Plane
The frontal plane is the ‘side-to-side’ plane of movement.
Some common Frontal Plane problems include:
- Dynamic Knee Valgus
- Pelvic Drop
Dynamic Valgus (or medial collapse of the knee) is a common issue we see in runners.
Excessive knocking in of the knee can lead to ligament injuries, accelerate meniscus as well as articular cartilage degeneration, and in younger runners it increases the risk for Patellofemoral pain and/or Patellar tendonitis. 23 24 25
Researchers have found that an increase in dynamic valgus of 10 degrees during the stance phase of running, resulted in a 45% increase in peak pressure within the knee. 26 Over time, excessive frontal plane movement at the knee may contribute to the onset of osteoarthritis. 27 28
If your knees touch at mid-stance (when one leg is swinging past the other) you likely have an issue here. We want to maintain a ‘window’ between the knees when parallel.
Strength training (especially the gluteal muscles) can have a big effect here.
Pelvic Drop is a very common frontal plane problem.

Minimal or no drop is ideal. 5-10 degrees is potentially a problem. > 10 degrees almost certainly should be addressed.
There is good research to indicate that excessive pelvic drop increases the risk of a number of injuries – in particular Patellofemoral pain – but also, medial knee ‘issues’, ITBS and LBP. 29 30 31 32
There are other considerations in the frontal plane as well – excessive calcaneal eversion, lateral trunk lean, cross-over gait pattern, etc… For those looking for an in-depth assessment of there gait, please click here for more information about our runner’s assessment, or contact us to set up an appointment.
Transverse Plane
The transverse plane is a ‘cross-section’. It is the rotational plane of movement for our trunk and limbs; And, it includes rotatory movements (such as ‘pronation’ and supination’) in the foot.
Some common Frontal Plane problems include:
- Excessive pronation
- Too little pronation
- Pelvic Rotation
Pronation is a word that has been given a bad rap. Pronation basically refers to the turning out of the heel and the flattening of the arch.
On one hand, excessive pronation is probably an issue. It has been associated with Achilles tendonopathy 33, patellofemoral pain 34 35 and medial tibial stress syndrome. 36 37 38 39
However, there is also a large pool of evidence that, the majority of the time, pronation is not necessarily a ‘dysfunction’ that needs to be resolved.
One particularly great study looking at this was a study on almost 1000 beginner runner. These ‘new’ runners were classified as ‘severe supinators’, ‘supinators’, ‘neutral’, ‘pronators’ and ‘severe pronators’. They were all given neutral shoes (the same shoe) and followed for a year. What they found was that the ‘Pronators’ group actually had a lower rate of injury (even though the shoes had no built in ‘correction’ 40 The authors concluded that “a pronated foot position is, if anything, an advantage with respect to running injuries.” The foot position that was associated with the lowest injury rates was ~ 7-10 deg of ‘eversion’ (pronation).
Multiple studies have investigated the link b/w pronation and injury rates only to show little>no link. 41 42 43
However, ‘severe’ pronation is likely a problem. Not olnly that, if a runner presents with an injury related to the mechanics of foot pronation (e.g. shin splints, Achilles Tendonitis, Plantar Fasciitis, etc) we must consider that their ‘ideal’ may not be the same as the average ‘ideal’ across a large population.
For much more detail on this topic, and the related conversation of ‘how to pick out the right running shoe’ – click here.
Pelvic Rotation is another common transverse plane problem found particularly in female runners. You can usually pick this on out your running partner. The pelvic is twisting side-to-side while running. Typically we expect to see more of a sinusoidal movement in the pelvic girdle. However, weakness of the trunk musculature, and/or tightness of the hip flexor muscles can lead to compensatory pelvic rotation.
Not only is this is a risk factor for LBP, but is very inefficient!
There are other considerations in the transverse plane as well – excessive trunk rotation, shoulder ‘cross-over’, femoral internal rotation, etc… For those looking for an in-depth assessment of there gait, please click here for more information about our runner’s assessment, or contact us to set up an appointment.
How to we ‘fix’ our mechanics
An overreliance on external support to improve running mechanics is likely misguided. Click here for a more detailed discussion on Running Shoes (and their limited ability to change our mechanics, or ‘control’ movement). One important message found in this discussion is that our bodies have a favored path of movement, and technology designed to modify this rarely works as well as we would like.
This idea is known as the “Preferred Movement Hypothesis”. This hypothesis was proposed by a group of running researchers from the university of Calgary. They attached sensors to the skeleton of runners (bone pins screwed into heel bones, shin bones and thigh bones!) and took data points while running in various shoes and inserts. What they found was that with changes in shoes and corrective inserts, the actual path of movement in space changed very little (and the changes they did observe was not consistent or predictable).
It appears that the runner will, regardless of the footwear, attempt to stay in the same (preferred) movement path. Muscle activity, to achieve this movement path, changes significantly with alterations in shoes and foot beds. Thus, the runner will feel different running in minimalist shoes vs. say a Hooka because it requires different muscles to achieve that ‘preferred movement path’ when running on different surfaces. Additionally, the amplitude of this movement path changes (for instance, when barefoot, the ankle will be dorsiflexed less at impact and the knee will be flexed more)… but the ‘path’ of movement will not change considerably.
So, we must recognize the limitations in the ability of shoes and/or orthotics to trues remodel our movement pathway when running.
But enough about what we can’t do… here’s what we can do:
First and foremost…“Get into shape in order to run”… not “Run to get into shape”
Building awareness and strength in the muscles that ‘control’ the frontal and transverse plane movements, so we can move more efficiently in the sagittal plane is important. These muscles do not build up on their own by simply running.
Also, strong gluts and calves may reduce some of the strain on the quadriceps (and therefore the knees) when running.
However, ‘building muscles up’, does NOT necessarily mean that your body will use them during running. 44 The research tells us that runners must purposefully ‘re-train’ their gait in addition to performing corrective strengthening exercises. Simple mirror training, mental imagery, or the use of low cost / easily accessible apps can be very effective here. 45
To develop an appropriate, progressive program based on your individual needs… Seek the advise of a Sports Physical Therapists with expertise in treating runners (and athletes that run!). Click here to request an appointment with one of our expert clinicians.
Some additional, easy to implement strategies:
1) Avoid excessive ‘contact time’. A ‘slow’ cadence is a common problem. Each runners ‘sweet spot’, with respect to turn over rate, is different. To effectively gauge whether your cadence is appropriate would require an individualized assessment. Many factors, such as body type, stride length, lower limb mobility, speed, terrain, etc… need to be considered. However, in general, middle to long distance runners with a cadence below 170 bbp are very likely spending too much time in contact with the ground. Research has shown that a 5% increase in cadence can reduce knee impact forces by almost 20%! 46 It also automatically reduces the tendency to ‘bounce’ and over stride.
2) Avoid excessive bounce. During a gait analysis, we would measure this. Again, many considerations go into determining the ‘right’ amount (or an ‘acceptable’ amount). However, you can ‘eyeball’ this one to get an idea if it’s a big problem. If you record yourself on a Treadmill and your just seems to bob up and down an awful lot, it’s likely a problem. Remember your are trying to go forward, not up! In stead of driving down into the ground as if you’re a rocket about to take off to the moon… drive the ground out behind you.
3) Avoid over striding. Make a conscious effort to not ‘stride out’ in front of the body much. By the time you ‘feel’ the ground reaction force up into your leg muscle, your trunk should be over the foot (not behind it). A slight trunk lean can help this (if you tend to run upright, or lean back), however, this should be subtle and is not the ‘right’ answer for everyone.
4) Attempt to land somewhat softly. Some runners run with too much accommodation in their legs. In other words, they bend their legs too much (to absorb impact) during load acceptance. So, I never tell entire populations to always try and run ‘softer’. However, if you are a runner that tends to ‘run stiff’… if you bend your knees less than ~ 20 degrees… if I can hear your strike on the treadmill from the other side of the gym, you would do well to attempt to back off the impact a bit. The command to ‘land softly’ has been shown to be an effective mental imagery in cueing the runner to attenuate shock more efficiently.
Avoid motion analysis software. There are apps out there that will tell you what is ‘off’ about your gait… DO NOT USE THESE. What is ‘right’ or not is based on way too many individual factors. There are plenty of ‘findings’ that are outside the ‘normal’ (or typical) range that are adaptive for the

runner (due to say flexibility impairments, or an old injury). If you try to ‘correct’ the finding, with out consideration for the underlying ‘cause’ or compensation, you could easily do more harm than good.
Last, but importantly… Avoid nonsense!
There is a lot out there. If your Physical Therapist or running coach has you doing ridiculous drills, blowing up balloons, or attempting downright dangerous drills – Find a New Resource.
This link is a fabulous resource for those looking to geek out on additional quality research (rather than internet hype) about running related injuries
Remember, running related injuries tend to be repetitive stress injuries. By the time you are feeling pain, this process has likely been ‘building up’ for some time. A little rest and Advil might make you feel a bit better, but it clearly does not resolve the underlying issue. Don’t rely on the same ‘fix’ that helped your buddy (his issue is likely not exactly the same as yours). Don’t rely on Google. Have someone who knows what they are talking about take a look at you!
Contact us here to request an appointment, or call a care coordinator at VASTA to set up an assessment today! 802-399-2244.
- Sporting Good Manufacturer’s Association. (2011). Sports, fitness, & recreational activities topline participation report 2011.
- Department of Health, Physical Activity, Health Improvement and Protection. (2011) Start Active, Stay Active.
- McDougall, C. (2009). Born to run: A hidden tribe, superathletes, and the greatest race the world has never seen. New York: Alfred A. Knopf.
- Bramble, D. M., & Lieberman, D. E. (2004). Endurance running and the evolution of Homo. Nature, 432(7015), 345-352.
- Arendse, R. E., Noakes, T. D., Azevedo, L. B., Romanov, N., Schwellnus, M. P., & Fletcher, G. (2004). Reduced eccentric loading of the knee with the pose running method. Medicine and science in sports and exercise, 36(2), 272-277.
- Goss DL, Gross MT: A review of mechanics and injury trends among various running styles. Army Med Dep J 2012;JulSep:62–71
- Pope, R. P. (1999). Prevention of pelvic stress fractures in female army recruits. Military medicine, 164(5), 370.
- Boden, B. P., Osbahr, D. C., & Jimenez, C. (2001). Low-risk stress fractures. The American journal of sports medicine, 29(1), 100-111.
- Goss DL, Gross MT: A review of mechanics and injury trends among various running styles. Army Med Dep J 2012;JulSep:62–71
- Diebal, A. R., Gregory, R., Alitz, C., & Gerber, J. P. (2012). Forefoot running improves pain and disability associated with chronic exertional compartment syndrome. The American journal of sports medicine, 40(5), 1060-1067.
- Zadpoor, A. A., & Nikooyan, A. A. (2011). The relationship between lower-extremity stress fractures and the ground reaction force: a systematic review. Clinical biomechanics, 26(1), 23-28.
- Pohl, M. B., Hamill, J., & Davis, I. S. (2009). Biomechanical and anatomic factors associated with a history of plantar fasciitis in female runners. Clinical Journal of Sport Medicine, 19(5), 372-376.
- Williams III, D. S., McClay, I. S., & Manal, K. T. (2000). Lower extremity mechanics in runners with a converted forefoot strike pattern. Journal of Applied Biomechanics, 16(2), 210-218.
- Perl, D. P., Daoud, A. I., & Lieberman, D. E. (2012). Effects of footwear and strike type on running economy. Med Sci Sports Exerc, 44(7), 1335-43.
- Kulmala, J. P., Avela, J. A. N. N. E., Pasanen, K. A. T. I., & Parkkari, J. A. R. I. (2013). Forefoot strikers exhibit lower running-induced knee loading than rearfoot strikers. Medicine & Science in Sports & Exercise, 45(12), 2306-2313.
- Shih, Y., Lin, K. L., & Shiang, T. Y. (2013). Is the foot striking pattern more important than barefoot or shod conditions in running?. Gait & posture, 38(3), 490-494.
- Murphy, K., Curry, E. J., & Matzkin, E. G. (2013). Barefoot running: does it prevent injuries?. Sports Medicine, 43(11), 1131-1138.
- Altman, A. R., & Davis, I. S. (2012). Barefoot running: biomechanics and implications for running injuries. Current sports medicine reports, 11(5), 244-250.
- Olin, E. D., & Gutierrez, G. M. (2013). EMG and tibial shock upon the first attempt at barefoot running. Human movement science, 32(2), 343-352.
- Altman, A. R., & Davis, I. S. (2012). Barefoot running: biomechanics and implications for running injuries. Current sports medicine reports, 11(5), 244-250.
- Goss DL, Gross MT: A review of mechanics and injury trends among various running styles. Army Med Dep J 2012;JulSep:62–71
- Schubert, A. G., Kempf, J., & Heiderscheit, B. C. (2014). Influence of stride frequency and length on running mechanics: a systematic review. Sports health, 6(3), 210-217.
- Stefanyshyn, D. J., Stergiou, P., Lun, V. M., Meeuwisse, W. H., & Worobets, J. T. (2006). Knee angular impulse as a predictor of patellofemoral pain in runners. The American journal of sports medicine, 34(11), 1844-1851.
- Stefanyshyn, D. J., Stergiou, P., Lun, V. M. Y., Meeuwisse, W. H., & Nigg, B. M. (1999, August). Knee joint moments and patellofemoral pain syndrome in runners part i: a case control study; part ii: a prospective cohort study. In Fourth Symposium on Footwear Biomechanics. Canmore, Alberta, Canada.
- Willy, R. W., Manal, K. T., Witvrouw, E. E., & Davis, I. S. (2012). Are mechanics different between male and female runners with patellofemoral pain?. Medicine and science in sports and exercise, 44(11), 2165.
- Huberti, H. H., & Hayes, W. C. (1984). Patellofemoral contact pressures. The influence of q-angle and tendofemoral contact. JBJS, 66(5), 715-724.
- Baliunas, A. J., Hurwitz, D. E., Ryals, A. B., Karrar, A., Case, J. P., Block, J. A., & Andriacchi, T. P. (2002). Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthritis and cartilage, 10(7), 573-579.
- Miyazaki, T., Wada, M., Kawahara, H., Sato, M., Baba, H., & Shimada, S. (2002). Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Annals of the rheumatic diseases, 61(7), 617-622.
- Willson, J. D., & Davis, I. S. (2008). Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clinical biomechanics, 23(2), 203-211.
- Noehren, B., Davis, I., & Hamill, J. (2007). ASB Clinical Biomechanics Award Winner 2006: Prospective study of the biomechanical factors associated with iliotibial band syndrome. Clinical biomechanics, 22(9), 951-956.
- Noehren, B., Pohl, M. B., Sanchez, Z., Cunningham, T., & Lattermann, C. (2012). Proximal and distal kinematics in female runners with patellofemoral pain. Clinical biomechanics, 27(4), 366-371.
- Noehren, B., Hamill, J., & Davis, I. (2013). Prospective evidence for a hip etiology in patellofemoral pain. Medicine and science in sports and exercise, 45(6), 1120-1124.
- Munteanu, S. E., & Barton, C. J. (2011). Lower limb biomechanics during running in individuals with achilles tendinopathy: a systematic review. Journal of foot and ankle research, 4(1), 15.
- Duffey, M. J., Martin, D. F., Cannon, D. W., Craven, T., & Messier, S. P. (2000). Etiologic factors associated with anterior knee pain in distance runners. Medicine and science in sports and exercise, 32(11), 1825-1832.
- Barton, C. J., Levinger, P., Menz, H. B., & Webster, K. E. (2009). Kinematic gait characteristics associated with patellofemoral pain syndrome: a systematic review. Gait & posture, 30(4), 405-416.
- Messier, S. P., & Pittala, K. A. (1988). Etiologic factors associated with selected running injuries. Medicine and Science in Sports and Exercise, 20(5), 501-505.
- Chuter, V. H., & de Jonge, X. A. J. (2012). Proximal and distal contributions to lower extremity injury: a review of the literature. Gait & posture, 36(1), 7-15.
- Pohl, M. B., Mullineaux, D. R., Milner, C. E., Hamill, J., & Davis, I. S. (2008). Biomechanical predictors of retrospective tibial stress fractures in runners. Journal of biomechanics, 41(6), 1160-1165.
- Raissi, G. R., Cherati, A. D., Mansoori, K. D., & Razi, M. D. (2009). The relationship between lower extremity alignment and Medial Tibial Stress Syndrome among non-professional athletes. BMC Sports Science, Medicine and Rehabilitation, 1(1), 11.
- Nielsen, R. O., Buist, I., Parner, E. T., Nohr, E. A., Sørensen, H., Lind, M., & Rasmussen, S. (2013). Foot pronation is not associated with increased injury risk in novice runners wearing a neutral shoe: a 1-year prospective cohort study. Br J Sports Med, bjsports-2013.
- Nielsen, R. O., Buist, I., Sørensen, H., Lind, M., & Rasmussen, S. (2012). Training errors and running related injuries: a systematic review. International journal of sports physical therapy, 7(1), 58.
- Nielsen, R. Ø., Parner, E. T., Nohr, E. A., Sørensen, H., Lind, M., & Rasmussen, S. (2014). Excessive progression in weekly running distance and risk of running-related injuries: an association which varies according to type of injury. journal of orthopaedic & sports physical therapy, 44(10), 739-747.
- Nigg, B. M. (2001). The role of impact forces and foot pronation: a new paradigm. Clinical journal of sport medicine, 11(1), 2-9.
- Willy, R. W., & Davis, I. S. (2011). The effect of a hip-strengthening program on mechanics during running and during a single-leg squat. Journal of orthopaedic & sports physical therapy, 41(9), 625-632.
- Willy, R. W., Scholz, J. P., & Davis, I. S. (2012). Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clinical Biomechanics, 27(10), 1045-1051.
- Heiderscheit, B. C., Chumanov, E. S., Michalski, M. P., Wille, C. M., & Ryan, M. B. (2011). Effects of step rate manipulation on joint mechanics during running. Medicine and science in sports and exercise, 43(2), 296.
