Tennis Elbow
What Is It?
Tennis Elbow (TE), also known as Lateral Epicondylalgia, is a repetitive stress injury effecting the muscles and tendons that attach to your lateral elbow. Extensor carpi radialis brevis and extensor digitorum communis are the two most commonly effected muscles. 1
The bottom of your arm bone (the humerus) has two epicondyles (or bumps). If you stand upright with your arms straight and palms forward, the ‘lateral epicondyle’ is the bump on the outside, about one fingers width above the elbow crease.
The pain associated with TE is typically felt directly over the epicondyle or just below in the tendons that attach to it.
Common pain-provoking activities include grasping a coffee mug, gripping the steering wheel, opening a jar, or performing activities with excessive vibration (ie operating power tools).
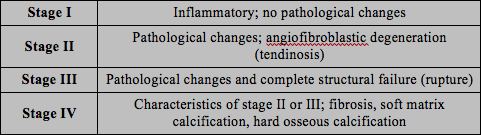
The science behind TE is complicated. Overuse and/or misuse may lead to micro-tearing of the tendons near the elbow attachment. This leads to weakness, a reduced ability to dissipate forces or transfer loads, and pain. Commonly, we see a ‘failed healing’ response with a sub-optimal cellular structure and alterations in gene-expression that promotes the production of pain generating substances. It has been proposed that the cellular response to repetitive microtrauma results in pathological tissue changes known as angiofibroblastic degeneration, or tendinosis. 2
Simply put, repetitive strain can result in pain and weakened tissue that time, by itself, does not resolve.
| Stages of Repetitive Microtrauma (Adapted from Nirschl, 1988) 3
Stage II changes are most commonly associated with sports participation and general over-use. |
Who Gets It?
TE a common musculoskeletal condition experienced by approximately 2.8% of the working population with individuals aged 45-54 being at the highest risk. 4 Men and Woman are affected almost equally.
Although commonly associated with tennis – the majority of those suffering from ‘Tennis Elbow’ are not raquet sports athletes. Manual laborers and smokers are at particular risk of developing this condition. The incidence of LE was found to be between 6.4-11.3% in individuals with repetitive, labor-intensive employment requirements. 5
Approximately 40% of tennis players will experience TE, commonly affecting those in their 30’s and 40’s.
Not surprisingly, as a repetitive stress injury, there is a link between playing time and incidence of TE. Specifically, playing > 2 hours/day doubles the risk for players over 40 and almost quadruples the risk for players under 40. 6 7
Interestingly, in an apparent contradiction to the idea that poor technique can lead to TE, studies have shown an increasing incidence of TE in Class A players when compared to Class C players. However, this is likely complicated by factors such as increased volume and/or intensity of play in higher-level athletes. Lending credence to the importance of form and technique is the finding that lower-class players have a higher recurrence.
How is it diagnosed?
The diagnoses of TE can be made clinically and diagnostic imaging is rarely indicated (i.e. X-rays, MRI, Ultrasound). 8
Clinical diagnoses are often made with reproduction of pain at the lateral epicondyle with at least one of the following activities:
|
Can I Prevent It?
There are a number of good prevention strategies to consider.
Equipment. Throw out your Jimmy Connors-era racquet and invest in something lightweight and younger than the Internet. Make sure the weight distribution in the racquet is proper. A racquet with a larger sweet spot may help. Make sure your handle size is appropriate for your grip.
Have a coach look at your mechanics! Seemingly ‘unrelated’ issues, such as keeping your knees bent during an overhead serve, can reduce strain to the shoulder and elbow.
Don’t skip the warm up. Get a structured warm-up plan in place and be disciplined.
Recovery! Make sure your training regimen includes a recovery plan (this is more than just days off).
Come into the season with some level of conditioning and avoid ramping up intensity and/or volume of play suddenly.
We blame ‘repetitive stress’ injuries on overuse, misuse or a combination of the two. The most common misuse is ramping up volume too quickly. Not, necessarily, to unrealistic levels, but simply at a rate that outpaces your body’s ability to ‘adapt’. Remember, your body will adapt to slow incremental increases in loads, but it will react to sudden increases in loads.
Misuse may refer to a wonky grip, or a hitch in your form due to an old injury.
Complex and explosive athletic movements require all parts of the biomechanical chain to be functioning at top level.
Tennis players of all ages and abilities would be well served to: 1) Get screened by a Sports Physical Therapists for common imbalances that predispose injury; 2) Participate in an off-season conditioning program to ensure the optimal functioning of the entire body; and 3) work with a tennis pro to correct issues with form.
What to Do About it Once it’s Here?
| A sudden onset of lateral elbow pain and/or TE may resolve on it’s own. However, for those with higher levels of pain, and/or those with > 6 weeks of pain, Physical Therapy intervention is strongly indicated.9 10 |
You’ve probably heard of the acronym R.I.C.E. (Rest, Ice, Compression, Elevation). Well, rehab professionals are now using another acronym – P.O.L.I.C.E. Protection, Optimal Loads (note – not necessarily rest!), Ice, Compression, and Elevation.
Frequently with TE, the I.C.E. is less important than the P.O.
While in rare and severe injuries full rest is required; more often, however, it can be counterproductive. Complete rest results in deconditioning of tissues, muscle atrophy, and stiffness. Defining ‘Optimal Loading’ for healing can prevent the athlete from ‘yo-yo’ing’ back and forth from ‘overuse’, to complete rest, and then back again. This is not a recipe for success (yet we see it all the time!).
‘Optimal Loads’ when battling TE includes two considerations: 1) Frequency, duration and intensity of play. Avoiding full fatigue during a single bout and ensure proper recovery between sessions; And 2) Introducing external loads (through resistance training) to strengthen the affected tissues between bouts of play. The goal here is to build resilience directly in the injured tissue, not just rest it. Consult with a Sports Physical Therapist for specific recommendations.
| The ‘optimal load’ depends on a number of factors – most significantly,
1) Time from initial Injury; and The ‘sweet spot’ with regards to exercise is a moving target and may include some low-level isometrics to apply very low loads (Isometrics also have an analgesic – pain reducing – effect of tendons. 11 12 13) or it may include some heavy, aggressive eccentric loading to trigger a ‘re-modeling’ effect (eccentric exercises have been shown to result in an increase in fibroblast activity, type I collagen formation, collagen organization and alignment). 14 |
Also, your physical therapist should look at your entire ‘biomechanical chain’ to make sure surrounding weakness is not increasing stress to the elbow.
Athletes with prior injuries, or weakness in core or shoulder girdle muscles are at increased risk of developing TE. 15
Significant differences in scapular (shoulder girdle) muscle strength and endurance have been reported in individuals with TE. 16 It is unknown whether these impairments predispose individuals to TE or if TE results in decreased muscle performance through to disuse and deconditioning as a result of fear avoidance (i.e. favoring the arm). 17 Regardless, the Sports Physical Therapists at VASTA have a variety of methods to treat these deficits and reduce your risk for future injuries.
‘Protection’ does not mean wrapping your arm in bubble wrap. Rather, it often refers to some modest equipment changes, grip modifications, the temporary use of a brace (such as a counterforce brace or strap), or temporarily modifying your game.
Some easy-to-follow advise that is appropriate for most people with TE would be to avoid obvious stressors throughout the day; Heavy gripping + twisting (e.g. opening a stuck jar), and lifting objects in a palm down position, especially with the elbow fully extended (e.g. pouring milk from a gallon jug) should be minimized.
If you find yourself popping a handful of Advil, slapping on some frozen peas and resolving to ‘rest’ your arm for the week – rethink your strategy! This may result in a decreased pain in the short-term, but it will not ‘fix’ the underlying pathology.
Additional Physical Therapy Options
Elbow mobilizations can provide immediate pain-relief and improvement in pain-free grip strength. 18
Instrument Assisted Soft Tissue Techniques can increased activity of Fibroblasts (the cells that make new collagen to heal the tendon) 19( Gehlsen et al 1993), improve collagen fiber ‘alignment’, resilience and help accelerate healing time 20 and Taping – Several taping methods have been shown to help reduce pain associated with TE and help maintain pain relief between Physical Therapy treatment sessions. 21 22
‘Low Level Laser’ Therapy (LLLT) has been found to be effective in managing pain and increasing grip-strength in individuals with LE. 23
How Long will I be Out?
If TE sidelines you, a prognosis for recovery is very difficult. TE appears to be a complex and multi-factorial issue.
Most athletes with TE should avoid corticosteroid injections as they lead to delayed healing and an increased risk of recurrence in the long-term. 24
If you are experiencing any signs or symptoms of Tennis Elbow and would like to consult with one of our Sports Physical Therapists – Request an Appointment Now or give us a call at 802.399.2244.
Tennis is a ‘lifetime’ sport, right? Let’s plan for the long-haul.
- Vicenzino B. Lateral epicondylalgia: a musculoskeletal physiotherapy perspective. Man Ther. 2003;8(2):66-79. “The cardinal physical signs of LE are pain to direct palpation over the lateral epicondyle and reproduction of pain and weakness during grip strength testing. Commonly, resisted contractions of the extensor muscles of the forearm, particularly the extensor carpi radialis brevis are also painful.”
- Kraushaar BS, Nirschl RP. Tendinosis of the elbow (Tennis elbow): Clinical features and findings of histological, immunohistochemical, and electron microscopy studies. J Bone Jt Surg Am Vol Boston. 1999;81(2):259-278. “The term angiofibroblastic tendinosis refers to the degenerative changes that occur when a tendon has failed to heal properly after an injury or after repetitive microtrauma resulting from overuse.”
- Nirschl RP. Prevention and treatment of elbow and shoulder injuries in the tennis player. Clin Sports Med. 1988;7(2):289-308.
- Shiri R, Viikari-Juntura E, Varonen H, Heliövaara M. Prevalence and determinants of lateral and medial epicondylitis: a population study. Am J Epidemiol. 2006;164(11):1065-1074. doi:10.1093/aje/kwj325. “The prevalence of lateral epicondylitis (definite or possible) was 2.8 percent…It was highest in subjects aged 45–54…”
- Kurppa K, Viikari-Juntura E, Kuosma E, Huuskonen M, Kivi P. Incidence of tenosynovitis or peritendinitis and epicondylitis in a meat-processing factory. Scand J Work Environ Health. 1991;17(1):32-37. “The food and textile industries show the highest rates for cases of tenosynovitis, peritendinitis, and epicondylitis…”
- Gruchow, William, and Douglas Pelletier. “An epidemiologic study of tennis elbow: Incidence, recurrence, and effectiveness of prevention strategies.” American Journal of Sports Medicine. 7.4 (1979): 234-238. “An epidemiologic study of the incidence and recurrence of tennis elbow among over 500 tennis players (278 men, 254 women; age range, 20 to 50 years) indicated that age and amount of playing time per day were contributing factors to the injury.”
- Tennis Elbow. Mayo Clinic Medical Information and Tools for Healthy Living – MayoClinic.com. 15 Oct. 2008. Web. 10 Oct. 2010. “While tennis elbow affects people of all ages, it’s most common in adults between the ages of 30 and 50.”
- Coombes BK, Bisset L, Vicenzino B. Management of Lateral Elbow Tendinopathy: One Size Does Not Fit All. J Orthop Sports Phys Ther. 2015;45(11):938-949. doi:10.2519/jospt.2015.5841. “While changes on imaging that are apparent in both affected and unaffected limbs require cautious interpretation, negative ultrasound findings can be used to confidently rule out LET as a diagnosis and prompt the clinician to consider other causes of elbow pain.”
- Coombes BK, Bisset L, Vicenzino B. Management of Lateral Elbow Tendinopathy: One Size Does Not Fit All. J Orthop Sports Phys Ther. 2015;45(11):938-949. doi:10.2519/jospt.2015.5841. “In patients with chronic LET, exercise has been shown to lead to greater and faster regression of pain,”
- Bisset L, Beller E, Jull G, Brooks P, Darnell R, Vicenzino B. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomised trial. BMJ. 2006;333(7575):939. doi:10.1136/bmj.38961.584653.AE. “An approach combining elbow manipulation and exercise has a superior benefit”
- Koltyn KF, Umeda M. Contralateral attenuation of pain after short-duration submaximal isometric exercise. J Pain 2007;8:887–92. “It is concluded that submaximal isometric exercise performed for 2 minutes resulted in ipsilateral and contralateral hypoalgesic responses.”
- Rio E, Kidgell D, Purdam C, et al. Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. British Journal of Sports Medicine. 2015;49(19):1277-1283. doi:10.1136/bjsports-2014-094386. “A single resistance training bout of isometric contractions reduced tendon pain immediately for at least 45 min postintervention and increased MVIC.”
- Rio E, Kidgell D, Moseley GL, et al. Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review. British Journal of Sports Medicine. September 2015:bjsports–2015–095215–9. doi:10.1136/bjsports-2015-095215) “Isometric exercise provided greater immediate analgesia and both protocols reduced pain significantly over the 4-week trial”
- Camargo PR, Alburquerque-Sendín F, Salvini TF. Eccentric training as a new approach for rotator cuff tendinopathy: Review and perspectives. World J Orthop. 2014;5(5):634-644. doi:10.5312/wjo.v5.i5.634. “eccentric training should be used aiming improvement of the tendon degeneration…”
- Day JM, Bush H, Nitz AJ, Uhl TL. Scapular muscle performance in individuals with lateral epicondylalgia. J Orthop Sports Phys Ther. 2015;45(5):414-24. “the weakness of the scapular musculature could be a result of LE.”
- Day JM, Bush H, Nitz AJ, Uhl LE. Scapular muscle performance in individuals with lateral epicondylalgia. J Orthop Sports Phys Ther. 2015;45(5):414-424. doi:10.2519/jospt.2015.5290. “…as the weakness of the scapular musculature could be a result of LE.”
- Alizadeh khaiyat O, Fisher AC, Kemp GJ, Vishwanathan K, Frostick SP. Upper limb muscle imbalance in tennis elbow: a functional and electromyographic assessment. J Orthop Res Off Publ Orthop Res Soc. 2007;25(12):1651-1657. doi:10.1002/jor.20458. “A global upper limb weakness exists in tennis elbow. This may be due to disuse and deconditioning syndrome caused by fear avoidance, and needs to be addressed in prevention and treatment. Activation imbalance among forearm muscles (reduced extensor carpi radialis activity) in tennis elbow, probably due to protective pain-related inhibition, could lead to a widespread upper limb muscle imbalance.”
- Vicenzino B, Cleland JA, Bisset L. Joint Manipulation in the Management of Lateral Epicondylalgia: A Clinical Commentary. J Man Manip Ther. 2007;15(1):50-56. “there is solid evidence to support the use of joint manipulations in the treatment of LE.”
- Davidson CJ, et al. Rat Tendon Morphologic and Functional Changes Resulting From Soft Tissue Mobilization. Med Sci Sports Exerc. 1997 mar;29(3):313-9. “…the findings of this study suggest that ASTM may promote healing via increased fibroblast recruitment.”
- Loghmani, T. Warden, S. Instrument-Assisted Cross-Fiber Massage Accelerates Knee Ligament Healing. J of Ortho & Sports Phys Ther. “Results indicate that IACFMtreated ligaments were 43% stronger, 40% stiffer, and able to absorb 57% more energy than contralateral, nontreated, injured ligaments at 4 weeks following injury.”
- Vicenzino B. Lateral epicondylalgia: a musculoskeletal physiotherapy perspective. Man Ther. 2003;8(2):66-79. “The cardinal physical signs of LE are pain to direct palpation over the lateral epicondyle and reproduction of pain and weakness during grip strength testing. Commonly, resisted contractions of the extensor muscles of the forearm, particularly the extensor carpi radialis brevis are also painful.”
- Amro A, Diener I, Bdair WO, Hameda IM, Shalabi AI, Ilyyan DI. The effects of Mulligan mobilisation with movement and taping techniques on pain, grip strength, and function in patients with lateral epicondylitis. Hong Kong Physiother J. 2010;28(1):19-23. doi:10.1016/j.hkpj.2010.11.004. “This study showed that the combination of Mulligan techniques with traditional treatment leads to better outcomes in treatment of lateral epicondylitis than traditional treatment alone.”
- Tumilty S, Munn J, McDonough S, Hurley DA, Basford JR, Baxter GD. Low Level Laser Treatment of Tendinopathy: A Systematic Review with Meta-analysis. Photomed Laser Surg. 2009;28(1):3-16. doi:10.1089/pho.2008.2470. “Low level laser treatment was potentially effective in treating tendinopathy using recommended doses.”
- Coombes BK, Bisset L, Brooks P, Khan A, Vicenzino B. Effect of Corticosteroid Injection, Physiotherapy, or Both on Clinical Outcomes in Patients With Unilateral Lateral Epicondylalgia: A Randomized Controlled Trial. JAMA. 2013;309(5):461-469. doi:10.1001/jama.2013.129. “Among patients with chronic unilateral lateral epicondylalgia, the use of corticosteroid injection vs placebo injection resulted in worse clinical outcomes after 1 year, and physiotherapy did not result in any significant differences.”