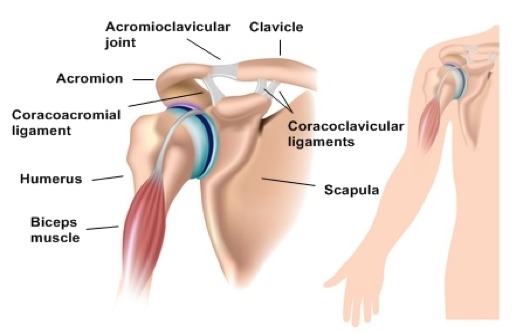
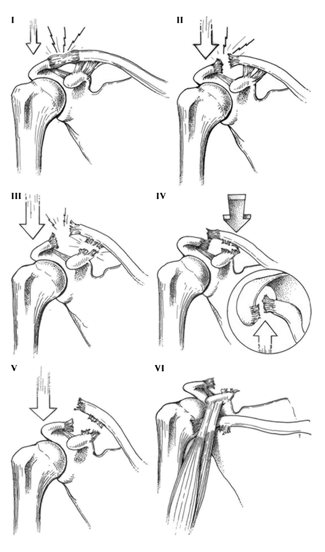
- Xinning Li, MD; Richard Ma, MD; Asheesh Bedi, MD; David M. Dines, MD; David W. Altchek, MD; Joshua S. Dines, MD. Current Concepts Review Management of Acromioclavicular Joint Injuries. J Bone Joint Surg Am, 2014 Jan 01; 96 (1): 73 -84. “Acromioclavicular joint injuries are common shoulder injuries that often result from direct trauma sustained during participation in contact sports. Anterior-to-posterior stability is provided by the acromioclavicular ligaments, while superior stability is provided by the coracoclavicular ligaments.”
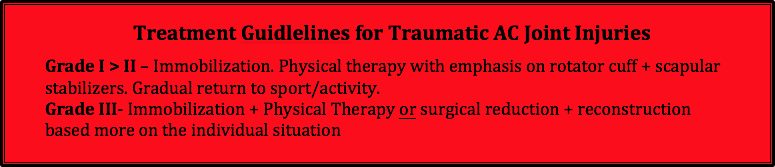
- Spencer EE Jr. Treatment of grade III acromioclavicular joint injuries: a systematic review. Clin Orthop Relat Res. 2007 Feb;455(Feb):38-44. “The three prospective, randomised studies all concluded that non-operative treatment was superior to surgery. Outcomes after surgery were no better than after non-surgical treatment, and surgery was associated with more complications, increased convalescence, and longer time away from work and sport.”
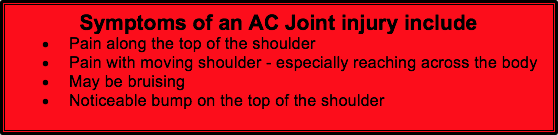
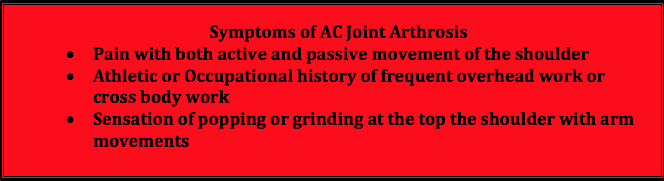
- Mall NA, Foley E, Chalmers PN, Cole BJ, Romeo AA, Bach BR Jr. Degenerative joint disease of the acromioclavicular joint: a review. Am J Sports Med. 2013;41(22):2684-2692. “Osteoarthritis of the acromioclavicular (AC) joint is a common condition causing anterior or superior shoulder pain, especially with overhead and cross-body activities.”
- Beim G. Acromioclavicular Joint Injuries. Journal of Athletic Training 2000;35(3):261–267 “…The most common events associated with AC injuries include contact sports such as hockey, rugby, and football. Webb and Bannister’4 noted a 45% incidence of AC injuries in first-class rugby players, and most did well with conservative treatment.”
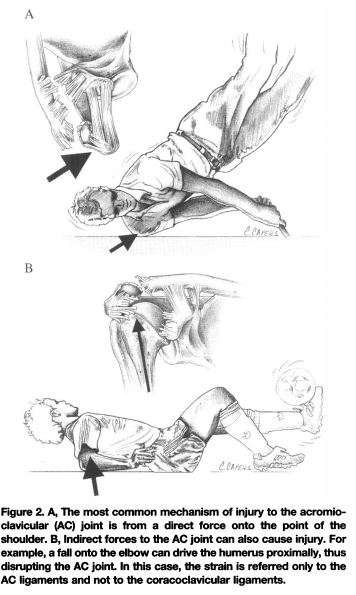
- Xinning Li, MD; Richard Ma, MD; Asheesh Bedi, MD; David M. Dines, MD; David W. Altchek, MD; Joshua S. Dines, MD. Current Concepts Review Management of Acromioclavicular Joint Injuries. J Bone Joint Surg Am, 2014 Jan 01; 96 (1): 73 -84. “Acromioclavicular joint injuries are among the most common shoulder girdle injuries in athletes and most commonly result from a direct force to the acromion with the arm in an adducted position.”
- Spencer EE Jr. Treatment of grade III acromioclavicular joint injuries: a systematic review. Clin Orthop Relat Res. 2007 Feb;455(Feb):38-44. “This review compared the efficacy of operative and non-operative treatment of grade III acromioclavicular separations. The author concluded that limited evidence suggests that non-operative treatments are superior. “
- Korsten K, Gunning AC, Leenen LPH. Operative or conservative treatment in patients with Rockwood type III acromioclavicular dislocation: a systematic review and update of current literature. International Orthopaedics. 2014;38(4):831-838. doi:10.1007/s00264-013-2143-7. “The objective and subjective shoulder function outcome was better in the operative group, especially in young adults, though the rate of complications and radiographic abnormalities were higher. The rehabilitation time was shorter in the conservative group, however the cosmetic outcome was worse.”
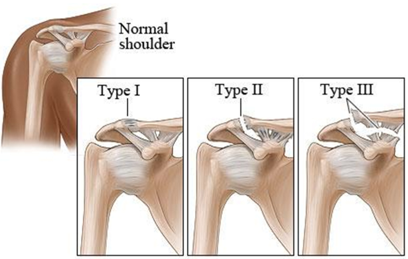
- Johnson L, Polson K, Reid D. Acromioclavicular joint separations grade I-III: best practice guidelines. Auckland: New Zealand Academy of Sport, 2011: 1-54. 8Johnson L, Polson K, Reid D. Acromioclavicular joint separations grade I-III: best practice guidelines. Auckland: New Zealand Academy of Sport, 2011: 1-54. “Historically, most studies have reported satisfactory results after nonoperative treatment for those with type I and II injuries”
- Xinning Li, MD; Richard Ma, MD; Asheesh Bedi, MD; David M. Dines, MD; David W. Altchek, MD; Joshua S. Dines, MD. Current Concepts Review Management of Acromioclavicular Joint Injuries. J Bone Joint Surg Am, 2014 Jan 01; 96 (1): 73 -84. “Type-I or type-II acromioclavicular joint injuries have been treated with sling immobilization, early shoulder motion, and physical therapy, with favorable outcomes.”
- Mikek M. Long-term shoulder function after type I and II acromioclavicular joint disruption. Am J Sports Med. 2008 Nov;36(11):2147-50. “Acromioclavicular joint separations are very common lesions, with the majority falling into Rockwood classification type I and II. It is generally agreed that conservative treatment of these injuries leads to good functional results, although there are some studies that suggest these injuries are associated with a high incidence of persistent symptoms.”
- Beim G. Acromioclavicular Joint Injuries. Journal of Athletic Training 2000;35(3):261–267 “…The most common events associated with AC injuries include contact sports such as hockey, rugby, and football. Webb and Bannister’4 noted a 45% incidence of AC injuries in first-class rugby players, and most did well with conservative treatment.”
- Johnson L, Polson K, Reid D. Acromioclavicular joint separations grade I-III: best practice guidelines. Auckland: New Zealand Academy of Sport, 2011: 1-54. “Historically, most studies have reported satisfactory results after nonoperative treatment for those with type I and II injuries”
- Xinning Li, MD; Richard Ma, MD; Asheesh Bedi, MD; David M. Dines, MD; David W. Altchek, MD; Joshua S. Dines, MD. Current Concepts Review Management of Acromioclavicular Joint Injuries. J Bone Joint Surg Am, 2014 Jan 01; 96 (1): 73 -84. “Type-I or type-II acromioclavicular joint injuries have been treated with sling immobilization, early shoulder motion, and physical therapy, with favorable outcomes.”
- Spencer EE Jr. Treatment of grade III acromioclavicular joint injuries: a systematic review. Clin Orthop Relat Res. 2007 Feb;455(Feb):38-44. “This review compared the efficacy of operative and non-operative treatment of grade III acromioclavicular separations. The author concluded that limited evidence suggests that non-operative treatments are superior. “
- Gstettner C, Tauber M, Hitzl W, Resch H. Rockwood type III acromioclavicular dislocation: surgical versus conservative treatment. J Shoulder Elbow Surg. 2008 Mar-Apr;17(2):220-5.” The best treatment for Rockwood type III injries is still controversial….24 patients who were treated surgically with a hook plate and 17 conservatively treated patients were examined iwht a mean follow-up of 34 months….In this study, better results were achieved by surgical treatment with the hook plate than by conservative treatment.”
- Spencer EE Jr. Treatment of grade III acromioclavicular joint injuries: a systematic review. Clin Orthop Relat Res. 2007 Feb;455(Feb):38-44. “This review compared the efficacy of operative and non-operative treatment of grade III acromioclavicular separations. The author concluded that limited evidence suggests that non-operative treatments are superior. “
- Gstettner C, Tauber M, Hitzl W, Resch H. Rockwood type III acromioclavicular dislocation: surgical versus conservative treatment. J Shoulder Elbow Surg. 2008 Mar-Apr;17(2):220-5.” The best treatment for Rockwood type III injries is still controversial….24 patients who were treated surgically with a hook plate and 17 conservatively treated patients were examined iwht a mean follow-up of 34 months….In this study, better results were achieved by surgical treatment with the hook plate than by conservative treatment.”
- Spencer EE Jr. Treatment of grade III acromioclavicular joint injuries: a systematic review. Clin Orthop Relat Res. 2007 Feb;455(Feb):38-44. “This review compared the efficacy of operative and non-operative treatment of grade III acromioclavicular separations. The author concluded that limited evidence suggests that non-operative treatments are superior. “
- Gstettner C, Tauber M, Hitzl W, Resch H. Rockwood type III acromioclavicular dislocation: surgical versus conservative treatment. J Shoulder Elbow Surg. 2008 Mar-Apr;17(2):220-5.” The best treatment for Rockwood type III injries is still controversial….24 patients who were treated surgically with a hook plate and 17 conservatively treated patients were examined iwht a mean follow-up of 34 months….In this study, better results were achieved by surgical treatment with the hook plate than by conservative treatment.”
- Spencer EE Jr. Treatment of grade III acromioclavicular joint injuries: a systematic review. Clin Orthop Relat Res. 2007 Feb;455(Feb):38-44. “This review compared the efficacy of operative and non-operative treatment of grade III acromioclavicular separations. The author concluded that limited evidence suggests that non-operative treatments are superior. “
- Gstettner C, Tauber M, Hitzl W, Resch H. Rockwood type III acromioclavicular dislocation: surgical versus conservative treatment. J Shoulder Elbow Surg. 2008 Mar-Apr;17(2):220-5.” The best treatment for Rockwood type III injries is still controversial….24 patients who were treated surgically with a hook plate and 17 conservatively treated patients were examined iwht a mean follow-up of 34 months….In this study, better results were achieved by surgical treatment with the hook plate than by conservative treatment.”
- Spencer EE Jr. Treatment of grade III acromioclavicular joint injuries: a systematic review. Clin Orthop Relat Res. 2007 Feb;455(Feb):38-44. “This review compared the efficacy of operative and non-operative treatment of grade III acromioclavicular separations. The author concluded that limited evidence suggests that non-operative treatments are superior. “
- Gstettner C, Tauber M, Hitzl W, Resch H. Rockwood type III acromioclavicular dislocation: surgical versus conservative treatment. J Shoulder Elbow Surg. 2008 Mar-Apr;17(2):220-5.” The best treatment for Rockwood type III injries is still controversial….24 patients who were treated surgically with a hook plate and 17 conservatively treated patients were examined iwht a mean follow-up of 34 months….In this study, better results were achieved by surgical treatment with the hook plate than by conservative treatment.”
- Beim G. Acromioclavicular Joint Injuries. Journal of Athletic Training 2000;35(3):261–267 “…The most common events associated with AC injuries include contact sports such as hockey, rugby, and football. Webb and Bannister’4 noted a 45% incidence of AC injuries in first-class rugby players, and most did well with conservative treatment.”
- Mall NA, Foley E, Chalmers PN, Cole BJ, Romeo AA, Bach BR Jr. Degenerative joint disease of the acromioclavicular joint: a review. Am J Sports Med. 2013;41(22):2684-2692. “Osteoarthritis of the acromioclavicular (AC) joint is a common condition causing anterior or superior shoulder pain, especially with overhead and cross-body activities.”
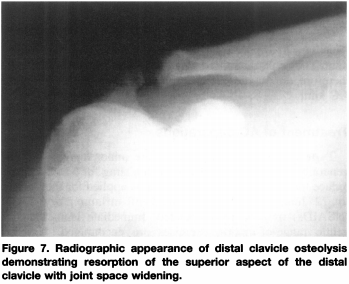
- Lervick GN. Direct Arthroscopic Distal Clavicle Resection: A Technical Review. The Iowa Orthopaedic Journal. 2005;25:149-156. “Treatment of isolated AC joint osteoarthritis is initially non-surgical. When such treatment fails to provide lasting relief, surgical treatment is warranted. Direct (superior) arthroscopic resection of the distal (lateral) end of the clavicle is a successful method of treating the condition, as well as other isolated conditions of the AC joint.”
- Mall NA, Foley E, Chalmers PN, Cole BJ, Romeo AA, Bach BR Jr. Degenerative joint disease of the acromioclavicular joint: a review. Am J Sports Med. 2013;41(22):2684-2692. “Osteoarthritis of the acromioclavicular (AC) joint is a common condition causing anterior or superior shoulder pain, especially with overhead and cross-body activities.”
- Beim G. Acromioclavicular Joint Injuries. Journal of Athletic Training 2000;35(3):261–267 “…The most common events associated with AC injuries include contact sports such as hockey, rugby, and football. Webb and Bannister’4 noted a 45% incidence of AC injuries in first-class rugby players, and most did well with conservative treatment.”
- Mall NA, Foley E, Chalmers PN, Cole BJ, Romeo AA, Bach BR Jr. Degenerative joint disease of the acromioclavicular joint: a review. Am J Sports Med. 2013;41(22):2684-2692. “Osteoarthritis of the acromioclavicular (AC) joint is a common condition causing anterior or superior shoulder pain, especially with overhead and cross-body activities.”
- Lervick GN. Direct Arthroscopic Distal Clavicle Resection: A Technical Review. The Iowa Orthopaedic Journal. 2005;25:149-156. “Treatment of isolated AC joint osteoarthritis is initially non-surgical. When such treatment fails to provide lasting relief, surgical treatment is warranted. Direct (superior) arthroscopic resection of the distal (lateral) end of the clavicle is a successful method of treating the condition, as well as other isolated conditions of the AC joint.”
- Mall NA, Foley E, Chalmers PN, Cole BJ, Romeo AA, Bach BR Jr. Degenerative joint disease of the acromioclavicular joint: a review. Am J Sports Med. 2013;41(22):2684-2692. “Osteoarthritis of the acromioclavicular (AC) joint is a common condition causing anterior or superior shoulder pain, especially with overhead and cross-body activities.”
- Mall NA, Foley E, Chalmers PN, Cole BJ, Romeo AA, Bach BR Jr. Degenerative joint disease of the acromioclavicular joint: a review. Am J Sports Med. 2013;41(22):2684-2692. “Osteoarthritis of the acromioclavicular (AC) joint is a common condition causing anterior or superior shoulder pain, especially with overhead and cross-body activities.”
- Lervick GN. Direct Arthroscopic Distal Clavicle Resection: A Technical Review. The Iowa Orthopaedic Journal. 2005;25:149-156. “Treatment of isolated AC joint osteoarthritis is initially non-surgical. When such treatment fails to provide lasting relief, surgical treatment is warranted. Direct (superior) arthroscopic resection of the distal (lateral) end of the clavicle is a successful method of treating the condition, as well as other isolated conditions of the AC joint.”
- Mall NA, Foley E, Chalmers PN, Cole BJ, Romeo AA, Bach BR Jr. Degenerative joint disease of the acromioclavicular joint: a review. Am J Sports Med. 2013;41(22):2684-2692. “Osteoarthritis of the acromioclavicular (AC) joint is a common condition causing anterior or superior shoulder pain, especially with overhead and cross-body activities.”
Additional Information
Contact Us Today
Phone: 802.399.2244
Fax: 802.497.2366
Get Started
VASTA Performance Training and Physical Therapy
358 Dorset Street
South Burlington, VT 05403
1185 Shelburne Rd
South Burlington, VT 05403
802-399-2244
80 S Main Street, Suite #7
Waterbury, VT 05676
802-882-8538
32 Cottonwood Drive
Suite 100
Williston, VT 05495
802-764-0046
5301 South Dixie Hwy
West Palm Beach, FL 33405
802-655-5100
South Burlington, VT 05403
1185 Shelburne Rd
South Burlington, VT 05403
802-399-2244
80 S Main Street, Suite #7
Waterbury, VT 05676
802-882-8538
32 Cottonwood Drive
Suite 100
Williston, VT 05495
802-764-0046
5301 South Dixie Hwy
West Palm Beach, FL 33405
802-655-5100





Share this entry