Meniscus Injuries
Meniscal injuries are the second most common injury to the knee with a prevalence of 12-14% and an incidence of 61/100,000 persons 1
In high school athletes, the meniscus is involved in 23% of all knee injuries with girls experiencing a higher injury rate compared to boys.2 As men age, their incidence increases and is most commonly seen between the ages of 21-30.3 Imaging evidence of a meniscal tear is observed in 35% of persons older than 50 years of age, with two thirds of these tears being asymptomatic.4 The prevalence increases in individuals who have an anterior cruciate ligament (ACL) deficient knee and if they are undergoing an ACL reconstruction or revision.5Ultimately, meniscal injuries can be observed throughout multiple age groups, all genders, and are more prevalent in girls ages 11-20, males ages 21-30, and in adults >50 years old who have been previously diagnosed with knee osteoarthritis.6 7
Anatomy of the Meniscus
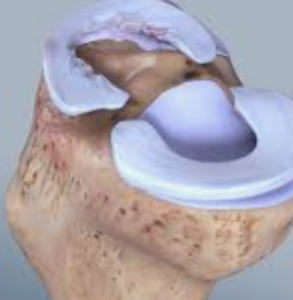
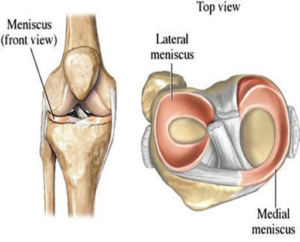 The meniscus is comprised of two parts, the medial and lateral meniscus. They each cover the superior (upper most) aspect of the tibia (shin bone) and are composed of wedge shaped fibrocartilage that is composed of up to 72% water.8
The meniscus is comprised of two parts, the medial and lateral meniscus. They each cover the superior (upper most) aspect of the tibia (shin bone) and are composed of wedge shaped fibrocartilage that is composed of up to 72% water.8
The lateral meniscus is smaller and more circular, it does not attach to any other ligaments of tissues within the joint. Whereas the medial meniscus is more crescent shaped, is larger, and attaches to the medial collateral ligament (MCL) in the knee. This attachment is important as it allows for the medial meniscus to play a larger role in stabilizing the knee during activity. When the ACL is injured the medial meniscus is recruited to help stabilize the knee. This recruitment can place the medial meniscus at risk of injury, as its function is not intended to stabilize the knee independently. 9 10
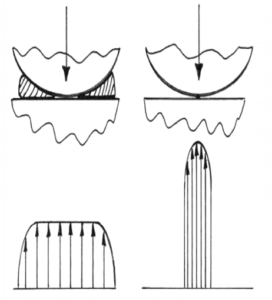
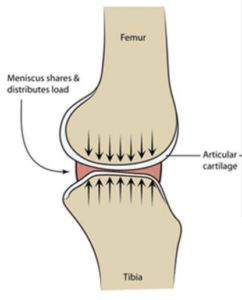 The role of the meniscus in the knee is highly complex. The primary function is to distribute stress across the knee during weight bearing and provide shock absorption. They also serve as a secondary joint stabilizer, provide articular cartilage nutrition and lubrication, facilitate joint gliding, and prevent hyperextension. 11Up to 40-60% of load in weight bearing is transmitted through the menisci. 12Regular loading of the joint allows for appropriate nutrition through compression and circulation of synovial fluid within the joint. If the contact area of the meniscus decreases via surgical intervention (meniscectomy), the compartment stress can increase up to 200-300% above normal. 13This concept must be considered when determining the appropriateness of surgical intervention.
The role of the meniscus in the knee is highly complex. The primary function is to distribute stress across the knee during weight bearing and provide shock absorption. They also serve as a secondary joint stabilizer, provide articular cartilage nutrition and lubrication, facilitate joint gliding, and prevent hyperextension. 11Up to 40-60% of load in weight bearing is transmitted through the menisci. 12Regular loading of the joint allows for appropriate nutrition through compression and circulation of synovial fluid within the joint. If the contact area of the meniscus decreases via surgical intervention (meniscectomy), the compartment stress can increase up to 200-300% above normal. 13This concept must be considered when determining the appropriateness of surgical intervention.
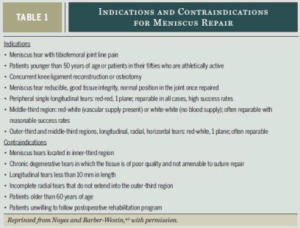
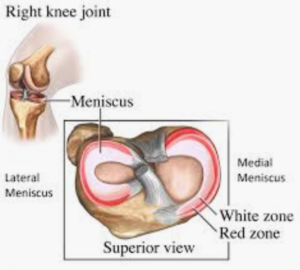 The blood supply for the meniscus changes throughout the surface area of the tibia. There are 3 zones within the meniscus that all experience different levels of vascularization. The outer 3rd is the red zone where if a meniscal tear is located here, it will likely respond to a surgical repair given its good healing potential. The middle 1/3rd is a red/white zone where vascularization is a mix, and the inner 1/3 has the poorest vascularization with the lowest healing potential.
The blood supply for the meniscus changes throughout the surface area of the tibia. There are 3 zones within the meniscus that all experience different levels of vascularization. The outer 3rd is the red zone where if a meniscal tear is located here, it will likely respond to a surgical repair given its good healing potential. The middle 1/3rd is a red/white zone where vascularization is a mix, and the inner 1/3 has the poorest vascularization with the lowest healing potential.
For this reason, tears isolated to this region are typically managed with PT or a simple surgical ‘debridement’ –or ‘clean up’ – to remove the damaged portion without any ‘repair’ or suturing. Therefore, the healing potential for the meniscus is highly dependent upon its location and is ultimately used to determine whether surgical intervention is indicated.14 15 16
Types of Tears
 Not only are there multiple locations where a tear can occur, there are multiple types of tears. Some are more commonly seen in acute traumatic tears where others are more prevalent in degenerative tears. Traumatic tears are often seen in young active participants and most commonly include the lateral meniscus (potentially with a simultaneous ACL injury secondary to their close proximity within the joint). A medial meniscus tear can be either traumatic or degenerative, commonly observed in athletes >30 y.o.17 and with chronic ACL injuries.18Degenerative tears are most commonly observed in males >40 y.o., and are atraumatic 19 Degenerative tears typically represent a gradual thinning or ‘wearing’ of the meniscus that eventually culminates in, what can be classified as, a tear – often without any known injury event. These injuriesmay be associated with a mechanical block to motion.20
Not only are there multiple locations where a tear can occur, there are multiple types of tears. Some are more commonly seen in acute traumatic tears where others are more prevalent in degenerative tears. Traumatic tears are often seen in young active participants and most commonly include the lateral meniscus (potentially with a simultaneous ACL injury secondary to their close proximity within the joint). A medial meniscus tear can be either traumatic or degenerative, commonly observed in athletes >30 y.o.17 and with chronic ACL injuries.18Degenerative tears are most commonly observed in males >40 y.o., and are atraumatic 19 Degenerative tears typically represent a gradual thinning or ‘wearing’ of the meniscus that eventually culminates in, what can be classified as, a tear – often without any known injury event. These injuriesmay be associated with a mechanical block to motion.20
Patterns of Tears
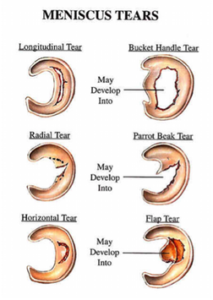 Tear patterns can also be classified as either traumatic or degenerative. Vertical longitudinal (bucket handle tear), radial, and oblique tears are often seen with trauma.21 Degenerative tears occur within multiple planes, initiating from the inner margin and travel outward. These can include horizontal and transverse tears, flap or complex tears, or meniscal maceration.22
Tear patterns can also be classified as either traumatic or degenerative. Vertical longitudinal (bucket handle tear), radial, and oblique tears are often seen with trauma.21 Degenerative tears occur within multiple planes, initiating from the inner margin and travel outward. These can include horizontal and transverse tears, flap or complex tears, or meniscal maceration.22
What causes a Meniscus to tear?
The primary traumatic mechanism for a meniscal tear involves twisting the knee with the knee flexed and the foot planted on the ground. The patient often reports onset during a cutting & pivoting activity often resulting in acute knee pain. They may report a sensation of “tearing”, feel a sharp pain immediately after the twisting mechanism, and may feel a “pop” while suddenly changing directions with or without contact.
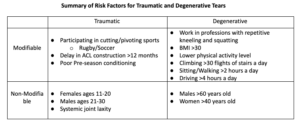
We previously discussed specific age groups and gender that may put an individual at an increased risk for a meniscal tear. Other risk factors associated with traumatic meniscal tears include participation in cutting and pivoting sports such as soccer and rugby23 . If there is a delay to ACL reconstruction of >12 months after an ACL rupture, this can be a risk factor for future medial meniscal tears.24 This is due to the medial meniscus acting as a secondary restraint for the ACL, therefore when the ACL is injured the meniscus then becomes the primary restraint for anterior to posterior translation of the tibia. When experiencing an acute ACL injury, the lateral meniscus is more likely to be seen in conjunction with the ACL tear secondary to the close approximation of these structures in the joint. (See our ACL info page for more details)
In degenerative tears, the risk increases in males who are older than 60 years old, who work in professions that require repetitive kneeling, squatting, and climbing more than 30 flights of stairs per day.25 26 Risk factors for tears in women include being greater then 40 years old with a body mass index (BMI) greater than 30, and with a lower physical activity level.27
Variables for both traumatic and degenerative tears can be modified in order to decrease the risk of a tear. These include specific sports participation, preseason conditioning, work activity level, BMI,
and length of time from initial ACL injury to reconstruction. Risk factors that are non-modifiable include age and gender.
Summary of Risk Factors for Traumatic and Degenerative Tears
A Physical Therapist, Athletic Trainer or Orthopedist can perform a specific examination in order to determine presence of a meniscal tear. A typical injury history may include a planting/twisting injury, possibly with an audible pop or a tearing sensation. Athletes may also experience occasional painful locking or catching in the knee. Swelling may occur, but can be delayed for 6-24 hours after injury.
How to clinically diagnose a tear?
Pain with forced hyperextension, maximal passive knee flexion and joint line tenderness are often present.
Two common tests performed include the McMurray’s Test and the Thessaly test. However, any one clinical test may have a limited value in current clinical practice, therefore clustering tests together can improve clinical accuracy. Joint line tenderness alone can demonstrate up to 74% accuracy for a medial meniscal tear and 96% for the lateral meniscus. When combined with a positive McMurray’s Test, pain with forced hyperextension and maximal knee flexion, as well as history of “catching” or “locking”, can improve the accuracy of a clinical examination to 99%. Magnetic Resonance Imaging (MRI) can also be used to confirm the presence of a meniscus tear. However, some studies point out limitations in accuracy – up to 94.5% accuracy, which is less than clinical testing 28 29 30 31 32 33– and high cost in questioning the value of regular MRI testing for suspected meniscus tear. Therefore, a well-trained clinician can be as accurate as an MRI. Given the high cost of an MRI and high rate of ‘false positives’, some suggest that an MRI should be reserved for traumatic tears in order to rule in/out concomitant injuries (such as an
ACL tear) in order to assist with the pre-operative planning and prognosis.34 An MRI may not be warranted for degenerative tears, as a thorough history and physical examination will
give you good diagnostic accuracy.
If it is not the meniscus, what else could it be?
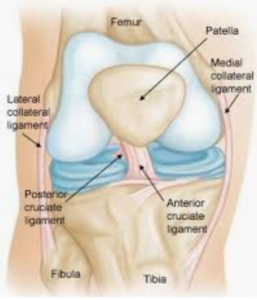 Other tissues that may be involved with a traumatic injury include the ligamentous and cartilaginous structures within the knee such as the ACL, MCL, LCL, and any osteochondral defect within the smooth cartilage at the end of each bone.
Other tissues that may be involved with a traumatic injury include the ligamentous and cartilaginous structures within the knee such as the ACL, MCL, LCL, and any osteochondral defect within the smooth cartilage at the end of each bone.
Also, your PT must be alert for the presence of any fracture associated with the lower extremity bones. The Ottawa knee rules can assist in determining when to order radiographs with an acute knee injury.
Osteoarthritis (OA) is a common differential diagnosis for older athletes as meniscal tears have a high prevalence within this population often making it difficult to determine whether symptoms are secondary to OA, meniscal tears, or both.35 Put another way, the presence of a meniscus tear upon imaging of a painful, arthritic knee, does not necessarily mean that the tear is causing the pain.
What are the surgical interventions?
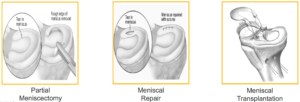
In the United States, 10% to 20% of all orthopedic surgeries consist of surgery to the meniscus with an estimated 850,000 patients each year.36 When determining appropriate interventions for \meniscal tears, the main goal is to normalize an individual’s function and quality of life first and foremost. Each surgical intervention looks to preserve as much of the meniscus as possible. The most common surgical interventions include arthroscopic partial meniscectomy (APM), meniscal repair
(MR), and meniscal allograft transplantation (MAT).
Arthroscopic Meniscectomy (AKA – Debridement or ‘Clean Up’)
 Over 465,000 persons undergo an APM annually in the US.37 APM is a procedure where the surgeon trims the torn meniscus back to a stable rim, removing loose fragments of cartilage and bone, but not penetrating the subchondral bone.38
Over 465,000 persons undergo an APM annually in the US.37 APM is a procedure where the surgeon trims the torn meniscus back to a stable rim, removing loose fragments of cartilage and bone, but not penetrating the subchondral bone.38
Some studies have shown that when comparing APM to non-operative treatment (physical therapy), there is no statistically significant difference between either groups with respect to functional improvement or pain relief over a period of 24 months.39
The limited usefulness of this procedure is particularly true in the case of degenerative meniscus tears. One systematic review of APM for degenerative meniscus tears reported minimal short-term improvement favoring arthroscopy compared to other treatments for pain; this ‘minimal improvement’ was then absent at 1 and 2 years. It has also been shown that patients who have non-operative management for a meniscus tear have similar to better outcomes in terms of strength and
perceived knee function in the short term and intermediate term compared to those who had APM.40 41Lastly, when looking at the cost-effectiveness of APM versus non-operative treatment, studies show APM is not economically effective and researchers suggest that the procedure should be reconsidered.42Overall, APM surgery may not be an effective treatment for degenerative tears – especially as the first or only intervention.
Meniscal Repair
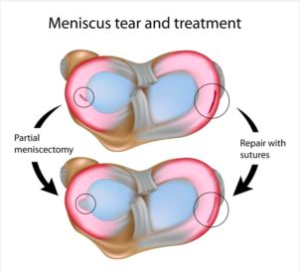 A meniscal repair is more commonly seen in the young, athletic population after sustaining a traumatic tear. The goal is to preserve healthy meniscus tissue. As previously discussed, the blood supply for the meniscus is best within the outer third portion of the meniscus. Therefore, repairs are most commonly seen in this outer region as it enables the best healing potential. However, some studies have demonstrated good clinical results in individuals >60 years who underwent a meniscal repair and in those <20 who had tears within the inner aspect of the meniscus. These studies recommend a meniscal repair whenever possible, regardless of location of tear and age.[note] Yoon KH, Park KH. Meniscal repair. Knee Surg Relat Res. 2014;26(2):68–76.[/note] Ultimately, the reparability depends on the vascularity, type of tear, chronicity and size of tear.
A meniscal repair is more commonly seen in the young, athletic population after sustaining a traumatic tear. The goal is to preserve healthy meniscus tissue. As previously discussed, the blood supply for the meniscus is best within the outer third portion of the meniscus. Therefore, repairs are most commonly seen in this outer region as it enables the best healing potential. However, some studies have demonstrated good clinical results in individuals >60 years who underwent a meniscal repair and in those <20 who had tears within the inner aspect of the meniscus. These studies recommend a meniscal repair whenever possible, regardless of location of tear and age.[note] Yoon KH, Park KH. Meniscal repair. Knee Surg Relat Res. 2014;26(2):68–76.[/note] Ultimately, the reparability depends on the vascularity, type of tear, chronicity and size of tear.
For an individual with an acute bucket handle meniscus tear that is adversely affecting or ‘blocking’ range of motion, surgery may be indicated immediately. In a systematic review, patients post meniscus repair had better self-reported knee function and less activity loss compared to those post meniscectomy.43Intuitively, non-operative treatment would be the cheaper and most conservative option however, it depends on the person, activity level, type and pattern of meniscus tear, chronicity of the tear, a patients’ symptoms, and patients’ beliefs.
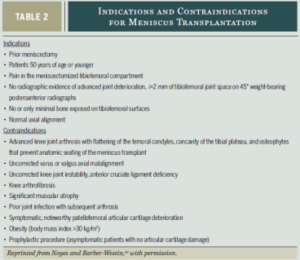
Meniscal Allograft Transplantation
A recently accepted option for select young symptomatic patient after a subtotal or total
meniscectomy is the meniscal allograft transplantation.44This procedure incorporates a meniscal implant from a cadaver or a synthetic material, with the main goal to preserve function of the menisci. This procedure would be indicated for an individual <50 years old with a prior meniscectomy, no evidence of osteoarthritis, and abnormal loading on the tibiofemoral joint surfaces.[note] Figueroa F, Figueroa D, Calvo R, Vaisman A, et al. Meniscus allograft transplantation: indications, techniques and outcomes. EFORT oen Rev[/note]The recovery for this procedure is more delayed when compared to a repair, and the return to sport recommendation has yet to be agreed upon.45
What would be my prognosis with these interventions?
Each surgical intervention presents with similar post-operative impairments. These primarily consist of swelling, decreased range of motion, abnormal joint function, asymmetry in surrounding muscle strength and mass (particularly of the quadriceps), impaired balance, abnormal gait as well as possible weight bearing restrictions.
 Physical therapy intervention will be required in order to address these impairments and allow patients to return to their prior level of function. However, the time it takes to return to that prior level of function can vary widely across each intervention.
Physical therapy intervention will be required in order to address these impairments and allow patients to return to their prior level of function. However, the time it takes to return to that prior level of function can vary widely across each intervention.
Multiple studies have been performed to determine outcomes of APM. One study demonstrated that APM can result in decreased muscle strength, balance, and poor patient reported outcomes.46 However, these impairments resolved within 2 years after surgery.47A different study demonstrated 12% quadriceps weakness in individuals up to 4 years after surgery.48 While a different study reported that perceived knee function and quality of life remain lower than healthy controls, also up to 4 years after an APM procedure.50 For women with previous knee injuries and lower preoperative fitness levels, post-operative recovery will likely be slower following APM.
As you can see, there is no clear answer to this question. There are many variables that can play a role in your recovery. It can depend on the location of tear, type of surgery, your age, activity level, gender, weight, pre-operative activity level, and so on. Therefore, it is extremely important to make an informed decision by utilizing evidence and the guidance of medical professionals to help determine the appropriate plan of care for you.
When would I choose non-operative treatment?
Surgery is not be recommended for everyone. Studies show that among patients with non-obstructive meniscal tears (e.g. no mechanical ‘locking’), physical therapy can be equal to APM for improving patient-reported knee function over a 24-month follow-up period.51 Based on these results, physical therapy may be considered an alternative to surgery for patients with non-obstructive meniscal tears.
Another study demonstrated that exercise therapy showed positive effects over surgery
in improving thigh muscle strength in the short term. These results should encourage clinicians and middle aged patients with degenerative meniscal tears to consider physical therapy as a treatment option.52
Patients who have non-operative management for meniscal tears have similar to better
outcomes in terms of strength and perceived knee function in the short term and intermediate term compared to those who had APM.53
When compared to no physical therapy at all, patients with degenerative tears demonstrated improvements in pain, muscle strength, and patient reported outcomes in those with exercise therapy compared to those without54– so, simply ‘giving it time is probably not the best route to take.
Ultimately, non-operative treatment can be an appropriate alternative option for treating a meniscus tear. In most cases, Physical Therapy should be trialed initially, especially if no meniscal obstruction or concomitant ACL tear is noted.
What would physical therapy intervention look like?
Physical therapy post-operatively initially concentrates on protection of the healing meniscus during the early rehabilitation process. The meniscus translates posteriorly with knee flexion and with associated weight-bearing, therefore range of motion and weight bearing restrictions are usually implemented. However, recent studies have demonstrated that early progressive active and passive knee motion, early progressive weight bearing and early progressive return to activity are necessary for optimal recovery.55
Post- and non-operative physical therapy would utilize supervised exercises targeting range of motion, strength training of the knee and hip muscles, and neuromuscular training. Neuromuscular training focuses on performing exercises to improve the efficiency of the nerves and muscles to communicate and react appropriately and efficiently during activity.
The use of neuromuscular electrical stimulation (NMES) should be provided very early on to increase quadriceps strength, functional performance and total knee function.56 Blood Flow Restriction training may also be used early on in rehab to minimize (or eliminate) quadriceps weakness during the ‘protective’ phase of recovery. Education should be provided in order to ensure independent and safe performance with all activities.
The intermediate phase of activity/rehab progresses all hip, core, and lower extremity strength, power, and endurance. Single leg exercises take precedence in order to progress towards symmetry. Proprioception and neuromuscular re-education techniques are utilized including low level agility, static and dynamic balance activities, full speed agility, and progression of plyometric training.
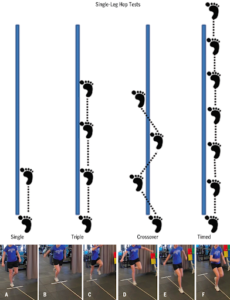 Lastly, when determining return to sport readiness, a patient will be tested and must pass all return to sport criteria. There is no single ‘gold standard’ test that will determine if a patient is ready to return safely. However, sports medicine professionals can utilize multiple tests/measures, observe quality of movement, and verify a patient’s confidence with activity in order to better determine readiness. A few tests that may be utilized (but do not constitute a comprehensive assessment) include single hop for distance, cross over hop for distance, triple hop for distance, and 6 m timed hop tests, to detect side to side asymmetries and determine readiness to RTS57
Lastly, when determining return to sport readiness, a patient will be tested and must pass all return to sport criteria. There is no single ‘gold standard’ test that will determine if a patient is ready to return safely. However, sports medicine professionals can utilize multiple tests/measures, observe quality of movement, and verify a patient’s confidence with activity in order to better determine readiness. A few tests that may be utilized (but do not constitute a comprehensive assessment) include single hop for distance, cross over hop for distance, triple hop for distance, and 6 m timed hop tests, to detect side to side asymmetries and determine readiness to RTS57
Ultimately, a patient should demonstrate full ROM, little to no swelling, quadriceps strength >90% (at least!) of the opposite leg, symmetry with hop testing >90% of the opposite leg, confidence progressively challenging rehabilitation tasks and with return to sports.58
Physical therapists need to be an advocate for their patients, therefore if any aspect of testing is not completed a patient should not be returning to sport.
Here at VASTA we pride ourselves in effectively and safely guiding our patients to return to their prior high-level of activity and performance. Click here to schedule an evaluation today. Those patients who have rehabilitated elsewhere are invited to have the sports medicine professionals at VASTA perform a comprehensive return to sports evaluation. Simply call our office at 802-399-2244
- Majewski M, Habelt S, Steinbrück K. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006;13:184-188.
- Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006–2010/2011. Med Sci Sports Exerc. 2013;45:462-469.
- Logerstedt D, Scalzitti D, Bennell K, Hinman R, et al. Knee pain and mobility impairments: meniscal and articular cartilage lesions revision 2018. J Orthop Sports Phys Ther. 2018;48(2): A1-A50.
- Katz J, Brophy R, Chaisson C, Chaves L, Cole B, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engk J Med. 2013:368;1675-1684.
- Majewski M, Habelt S, Steinbrück K. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006;13:184-188. knee.2006.01.005.
- Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006–2010/2011. Med Sci Sports Exerc. 2013;45:462-469.
- Katz J, Brophy R, Chaisson C, Chaves L, Cole B, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engk J Med. 2013:368;1675-1684.
- Fox, A. J., Wanivenhaus, F. , Burge, A. J., Warren, R. F. and Rodeo, S. A. (2015), The human meniscus: A review of anatomy, function, injury, and advances in treatment. Clin. Anat., 28: 269-287.
- Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006–2010/2011. Med Sci Sports Exerc. 2013;45:462-469.
- Brindle T, Nyland J, Johnson DL. The meniscus: review of basic principles with application to surgery and rehabilitation. J Athl Train. 2001;36:160-169.
- Fox, A. J., Wanivenhaus, F. , Burge, A. J., Warren, R. F. and Rodeo, S. A. (2015), The human meniscus: A review of anatomy, function, injury, and advances in treatment. Clin. Anat., 28: 269-287.
- Fox, A. J., Wanivenhaus, F. , Burge, A. J., Warren, R. F. and Rodeo, S. A. (2015), The human meniscus: A review of anatomy, function, injury, and advances in treatment. Clin. Anat., 28: 269-287.
- Fox, A. J., Wanivenhaus, F. , Burge, A. J., Warren, R. F. and Rodeo, S. A. (2015), The human meniscus: A review of anatomy, function, injury, and advances in treatment. Clin. Anat., 28: 269-287.
- Brindle T, Nyland J, Johnson DL. The meniscus: review of basic principles with application to surgery and rehabilitation. J Athl Train. 2001;36:160-169.
- Snoeker BA, Bakker EW, Kegel CA, Lucas C. Risk factors for meniscal tears: a systematic review including meta-analysis. J Orthop Sports Phys Ther. 2013;43:352-367.
- Greis P, Bardana D, Holmstrom M, et al. Meniscal injury: I. basic science and evaluation. JAAOS. 10 (3): 168-176, May-June 2002
- Yeh PC, Starkey C, Lombardo S, Vitti G, Kharrazi FD. Epidemiology of isolated meniscal injury and its effect on performance in athletes from the National Basketball Association. Am J Sports Med. 2012;40:589-594.
- Fox, A. J., Wanivenhaus, F. , Burge, A. J., Warren, R. F. and Rodeo, S. A. (2015), The human meniscus: A review of anatomy, function, injury, and advances in treatment. Clin. Anat., 28: 269-287.
- Fox, A. J., Wanivenhaus, F. , Burge, A. J., Warren, R. F. and Rodeo, S. A. (2015), The human meniscus: A review of anatomy, function, injury, and advances in treatment. Clin. Anat., 28: 269-287.
- Fox, A. J., Wanivenhaus, F. , Burge, A. J., Warren, R. F. and Rodeo, S. A. (2015), The human meniscus: A review of anatomy, function, injury, and advances in treatment. Clin. Anat., 28: 269-287.
- Englund M, Guermazi A, Lohmander SL. The role of the meniscus in knee osteoarthritis: a cause or consequence? Radiol Clin North Am. 2009;47:703-712.
- Englund M, Guermazi A, Lohmander SL. The role of the meniscus in knee osteoarthritis: a cause or consequence? Radiol Clin North Am. 2009;47:703-712.
- Snoeker BA, Bakker EW, Kegel CA, Lucas C. Risk factors for meniscal tears: a systematic review including meta-analysis. J Orthop Sports Phys Ther. 2013;43:352-367.
- Logerstedt D, Scalzitti D, Bennell K, Hinman R, et al. Knee pain and mobility impairments: meniscal and articular cartilage lesions revision 2018. J Orthop Sports Phys Ther. 2018;48(2): A1-A50.
- Logerstedt D, Scalzitti D, Bennell K, Hinman R, et al. Knee pain and mobility impairments: meniscal and articular cartilage lesions revision 2018. J Orthop Sports Phys Ther. 2018;48(2): A1-A50.
- Snoeker BA, Bakker EW, Kegel CA, Lucas C. Risk factors for meniscal tears: a systematic review including meta-analysis. J Orthop Sports Phys Ther. 2013;43:352-367.
- Hwang BY, Kim SJ, Lee SW, et al. Risk factors for medial meniscus posterior root tear. Am J Sports Med. 2012;40:1606-1610.
-
- Arroll B, Robb G, Sutich E, et al. The Diagnosis and Management of Soft Tissue Knee Injuries: Internal Derangements. Wellington, New Zealand: New Zealand Guidelines Group; 2003.
- Bansal P, Deehan DJ, Gregory RJ. Diagnosing the acutely locked knee. Injury. 2002;33:495-498.
- Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85-A suppl 2:58-69.
- Hegedus EJ, Cook C, Hasselblad V, Goode A, McCrory DC. Physical examination tests for assessing a torn meniscus in the knee: a systematic review with meta-analysis. J Orthop Sports Phys Ther. 2007;37:541-550.
- Lowery DJ, Farley TD, Wing DW, Sterett WI, Steadman JR. A clinical composite score accurately detects meniscal pathology. Arthroscopy. 2006;22:1174-1179.
Ryzewicz M, Peterson B, Siparsky PN, Bartz RL. The diagnosis of meniscus tears: the role of MRI and clinical examination. Clin Orthop Relat Res. 2007;455:123-133.
- Logerstedt D, Scalzitti D, Bennell K, Hinman R, et al. Knee pain and mobility impairments: meniscal and articular cartilage lesions revision 2018. J Orthop Sports Phys Ther. 2018;48(2): A1-A50.
- Katz J, Brophy R, Chaisson C, Chaves L, Cole B, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engk J Med. 2013:368;1675-1684.
- Logerstedt D, Scalzitti D, Bennell K, Hinman R, et al. Knee pain and mobility impairments: meniscal and articular cartilage lesions revision 2018. J Orthop Sports Phys Ther. 2018;48(2): A1-A50.
- Katz J, Brophy R, Chaisson C, Chaves L, Cole B, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engk J Med. 2013:368;1675-1684
- Thorlund JB, Juhl CB, Roos EM, Lohmander LS. Arthroscopic surgery for degenerative knee: systematic review and meta-analysis of benefits and harms. Br J Sports Med. 2015;49:1229 1235.
- Thorlund JB, Juhl CB, Roos EM, Lohmander LS. Arthroscopic surgery for degenerative knee: systematic review and meta-analysis of benefits and harms. Br J Sports Med. 2015;49:1229 1235.
- Logerstedt D, Scalzitti D, Bennell K, Hinman R, et al. Knee pain and mobility impairments: meniscal and articular cartilage lesions revision 2018. J Orthop Sports Phys Ther. 2018;48(2): A1-A50.
- Rongen JJ, Royers MM, Van Tienen TG, Buma P. Hannink G. Increased risk for knee replacement surgery after arthroscopic surgery for degenerative meniscal tears: a multi-center longitudinal observational study using data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2017; 25:25-29
- Marsh JD, Birmingham TB, Giffin JR, et al. Cost-effectiveness analysis of arthroscopic surgery compared with non-operative management for osteoarthritis of the knee. BMJ Open. 2016;6(1):e009949. Published 2016 Jan 12. doi:10.1136/bmjopen-2015-009949
- Xu C, Zhao J. A meta-analysis comparing meniscal repair with meniscectomy in the treatment of meniscal tears: the more meniscus, the better outcome? Knee Surg Sports Traumatol Arthrosc. 2015;23:164-170.
- Noyes F, Heckmann T, Barber-Westin S. Meniscus repair and transplantation: a comprehensive update. JOSPT. 2012;42(3):274-290
- Figueroa F, Figueroa D, Calvo R, Vaisman A, et al. Meniscus allograft transplantation: indications, techniques and outcomes. EFORT oen Rev
- Al-Dadah O, Shepstone L, Donell ST. Proprioception following partial meniscectomy in stable knees. Knee Surg Sports Traumatol Arthrosc. 2011;19:207-213.
- Al-Dadah O, Shepstone L, Donell ST. Proprioception following partial meniscectomy in stable knees. Knee Surg Sports Traumatol Arthrosc. 2011;19:207-213.
- Hall M, Juhl CB, Lund H, Thorlund JB. Knee extensor muscle strength in middle-aged and older individuals undergoing arthroscopic partial meniscectomy: a systematic review and meta-analysis. Arthritis Care Res (Hoboken). 2015;67:1289-1296.
- Thorlund JB, Aagaard P, Roos EM. Muscle strength and functional performance in patients at high risk of knee osteoarthritis: a follow-up study. Knee Surg Sports Traumatol Arthrosc. 2012;20:1110-1117.[/note/] Ultimately, these studies do not demonstrate excellent short term outcomes for APM.
When comparing a meniscus repair to APM, young patients who undergo a repair have similar to better perceived long term knee function, less activity loss, and higher rates of return to activity compared to those with an APM.49Logerstedt D, Scalzitti D, Bennell K, Hinman R, et al. Knee pain and mobility impairments: meniscal and articular cartilage lesions revision 2018. J Orthop Sports Phys Ther. 2018;48(2): A1-A50.
- Van De Graaaf V, Noorduyn J, Willigenburg N,Butter I, et al. Effect of early surgery vs physical therapy on knee function among patients with nonobstructive meniscal tears: the escapre randomized clilnical trial. JAMA 2018; 12: 1328-1337
- Kise NJ, Risberg MA, Stensrud S, Ranstam J, et al. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomized controlled trial with two year follow-up. BMJ. 2016:354-374
- Logerstedt D, Scalzitti D, Bennell K, Hinman R, et al. Knee pain and mobility impairments: meniscal and articular cartilage lesions revision 2018. J Orthop Sports Phys Ther. 2018;48(2): A1-A50.
- Logerstedt D, Scalzitti D, Bennell K, Hinman R, et al. Knee pain and mobility impairments: meniscal and articular cartilage lesions revision 2018. J Orthop Sports Phys Ther. 2018;48(2): A1-A50.
- Logerstedt D, Scalzitti D, Bennell K, Hinman R, et al. Knee pain and mobility impairments: meniscal and articular cartilage lesions revision 2018. J Orthop Sports Phys Ther. 2018;48(2): A1-A50.
- Logerstedt D, Scalzitti D, Bennell K, Hinman R, et al. Knee pain and mobility impairments: meniscal and articular cartilage lesions revision 2018. J Orthop Sports Phys Ther. 2018;48(2): A1-A50.
- Logerstedt D, Scalzitti D, Bennell K, Hinman R, et al. Knee pain and mobility impairments: meniscal and articular cartilage lesions revision 2018. J Orthop Sports Phys Ther. 2018;48(2): A1-A50.
- Adams d, Logerstedt D, Hunter-Giordano A, Axe M, et al. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. JOSPT. 2012; 42:601-614
